Form 10-K Cara Therapeutics, Inc. For: Dec 31
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM
| ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
FOR THE FISCAL YEAR ENDED
OR
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
COMMISSION FILE NUMBER:
(Exact name of registrant as specified in its charter)
| ||
(State or other jurisdiction of | (I.R.S. Employer |
| ||
(Address of registrant’s principal executive offices) | (Zip Code) |
Registrant’s telephone number, including area code: (
Securities registered pursuant to Section 12(b) of the Act:
Title of each class | Trading Symbol | Name of each exchange on which registered |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ◻
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ◻
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days.
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T (§ 232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit such files).
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer”, “accelerated filer”, “smaller reporting company”, and “emerging growth company” in Rule 12b-2 of the Exchange Act.
☒ | Accelerated filer | ☐ | |||
Smaller Reporting Company | |||||
Non-accelerated filer | ☐ | Emerging growth company |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ◻
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report.
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes
The aggregate market value of the registrant’s Common Stock (the only common equity of the registrant) held by non-affiliates, based on the closing sales price of the stock on the Nasdaq Global Market for the last business day of the registrant’s most recently completed second fiscal quarter, was $
The number of shares outstanding of the registrant’s Common Stock, par value $0.001 per share, as of February 24, 2022 was
Documents Incorporated By Reference
Portions of the registrant’s Proxy Statement for its 2022 Annual Meeting of Stockholders, to be filed with the Securities and Exchange Commission no later than 120 days after December 31, 2021, are incorporated by reference in Part III of this Annual Report on Form 10-K.
CARA THERAPEUTICS, INC.
2021 ANNUAL REPORT ON FORM 10-K
TABLE OF CONTENTS
PART I
In this Annual Report on Form 10-K, the terms “we,” “us” and “our” refer to Cara Therapeutics, Inc.
Cautionary Note Regarding Forward-Looking Statements
This Annual Report on Form 10-K contains forward-looking statements, within the meaning of the Private Securities Litigation Reform Act of 1995, that involve substantial risks and uncertainties. The forward-looking statements are contained principally in the sections of this Annual Report on Form 10-K titled “Risk Factors,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and “Business,” but are also contained elsewhere in this Annual Report on Form 10-K. In some cases, you can identify forward-looking statements by the words “aim”, “anticipate,” “believe,” “continue,” “could,” “estimate,” “expect,” “intend,” “may,” “might,” “objective,” “ongoing,” “plan,” “predict,” “project,” “potential,” “seek,” “should,” “will,” or “would,” and or the negative of these terms, or other comparable terminology intended to identify statements about the future. These statements involve known and unknown risks, uncertainties and other factors that may cause our actual results, levels of activity, performance or achievements to be materially different from the information expressed or implied by these forward-looking statements. Although we believe that we have a reasonable basis for each forward-looking statement contained in this Annual Report on Form 10-K, we caution you that these statements are based on a combination of facts and factors currently known by us and our expectations of the future, about which we cannot be certain.
The forward-looking statements in this Annual Report on Form 10-K include, among other things, statements about:
| ● | our ability to commercialize KORSUVATM (difelikefalin) injection, or KORSUVA injection, including the timing of additional regulatory submissions and approvals, and execute on our marketing plans for any other drugs or indications that may be approved in the future; |
| ● | our ability to obtain and maintain coverage and adequate reimbursement for KORSUVA injection; |
| ● | the performance of our current and future collaborators and licensees, including Vifor Fresenius Medical Care Renal Pharma Ltd., or VFMCRP, Vifor (International) Ltd., or Vifor, Maruishi Pharmaceuticals Co. Ltd., or Maruishi, and Chong Kun Dang Pharmaceutical Corp., or CKDP, as well as sub-licensees, including Kissei Pharmaceutical Co. Ltd., or Kissei, and our ability to maintain such collaborations; |
| ● | risks that KORSUVA injection revenue, expenses and costs may not be as expected; |
| ● | the performance of third-party manufacturers and clinical research organizations, or CROs; |
| ● | risks relating to KORSUVA injection’s market acceptance, competition, reimbursement and regulatory actions; |
| ● | the size and growth of the potential markets for pruritus management, including chronic kidney disease associated pruritus, or CKD-aP, in hemodialysis and non-dialysis markets, chronic liver disease associated pruritus, or CLD-aP, pruritus associated with atopic dermatitis, or AD-aP, and pruritus associated with notalgia paresthetica, or NP, markets; |
| ● | the success and timing of our clinical trials and reporting of our results from these trials, including our clinical trial programs for Oral KORSUVA (difelikefalin) in CKD-aP, CLD-aP, AD-aP, and NP; |
| ● | our plans to develop and commercialize Oral KORSUVA (difelikefalin) and any future product candidates; |
| ● | the potential results of ongoing and planned preclinical studies and clinical trials and future regulatory and development milestones for our product candidates; |
1
| ● | the rate and degree of market acceptance of any other future approved products; |
| ● | our ability to obtain and maintain additional regulatory approval of our product candidates, and the labeling under any approval we may obtain; |
| ● | the anticipated use of Enteris Biopharma, Inc.’s, or Enteris’s, Peptelligence® technology to develop, manufacture and commercialize Oral KORSUVA (difelikefalin); |
| ● | our ability to establish additional collaborations for our product candidates; |
| ● | the continued service of our key scientific or management personnel; |
| ● | our ability to establish commercialization and marketing capabilities for any other future approved products; |
| ● | regulatory developments in the United States and foreign countries; |
| ● | our ability to obtain and maintain coverage and adequate reimbursement from third-party payers for any other future approved products; |
| ● | our planned use of our cash and cash equivalents and marketable securities and the clinical milestones we expect to fund with such proceeds; |
| ● | the accuracy of our estimates regarding expenses, future revenues and capital requirements; |
| ● | our ability to obtain funding for our operations; |
| ● | our ability to obtain and maintain intellectual property protection for our product candidates and our ability to operate our business without infringing on the intellectual property rights of others; |
| ● | the success of competing drugs that are or may become available; and |
| ● | the potential effects of the ongoing COVID-19 pandemic on our business, operations and clinical development and regulatory timelines and plans as well as commercial and clinical drug supply chain continuity and the commercial launch of KORSUVA injection. |
You should refer to Part I Item 1A. “Risk Factors” of this Annual Report on Form 10-K for a discussion of material factors that may cause our actual results to differ materially from those expressed or implied by our forward-looking statements. As a result of these factors, we cannot assure you that the forward-looking statements in this Annual Report on Form 10-K will prove to be accurate. Furthermore, if our forward-looking statements prove to be inaccurate, the inaccuracy may be material. In light of the significant uncertainties in these forward-looking statements, you should not regard these statements as a representation or warranty by us or any other person that we will achieve our objectives and plans in any specified time frame or at all. We undertake no obligation to publicly update any forward-looking statements, whether as a result of new information, future events or otherwise, except as required by law.
You should read this Annual Report on Form 10-K and the documents that we reference in this Annual Report on Form 10-K and have filed as exhibits to this Annual Report on Form 10-K completely and with the understanding that our actual future results may be materially different from what we expect. We qualify all of our forward-looking statements by these cautionary statements.
2
Risk Factors Summary
Investing in our common stock involves a high degree of risk because our business is subject to numerous risks and uncertainties, as fully described below. The principal factors and uncertainties that make investing in our common stock risky include, among others:
| ● | We are substantially dependent on the success of our product and product candidates. If we are unable to successfully complete clinical development, obtain additional regulatory approvals and commercialize our product and product candidates, or experience significant delays in doing so, our business will be materially harmed. |
| ● | We rely, and expect to continue to rely, on third parties to conduct our preclinical studies and clinical trials, and those third parties may not perform satisfactorily, including failing to meet deadlines for the completion of such trials. |
| ● | If the manufacturers upon whom we rely fail to produce our products or product candidates in the volumes that we require on a timely basis, or to comply with stringent regulations applicable to pharmaceutical drug manufacturers, we may face delays in the development and commercialization of, or be unable to meet demand for, our products and may lose potential revenues. |
| ● | Even if we obtain additional regulatory approvals for our product candidates, they may never be successfully launched or become profitable, in which case our business, prospects, operating results and financial condition may be materially harmed. |
| ● | If we or our collaborators are unable to establish effective marketing and sales capabilities, or if we are unable to enter into or maintain agreements with third parties to market and sell our products and product candidates, if they are approved, we may be unable to generate product revenues. |
| ● | Any collaboration arrangements that we are a party to, such as our collaboration with Vifor Pharma, or may enter into in the future may not be successful, which could adversely affect our ability to develop and commercialize our product candidates. |
| ● | We face significant competition from other pharmaceutical and biotechnology companies, academic institutions, government agencies and other research organizations. Our operating results will suffer if we fail to compete effectively. |
| ● | To the extent that KORSUVA injection, or our product candidates, if approved, do not achieve broad market acceptance, the revenues that we generate from sales will be limited. |
| ● | Our business, operations and clinical development and regulatory timelines and plans have been, and could continue to be, adversely affected by the effects of health epidemics, including the ongoing COVID-19 pandemic. |
| ● | The regulatory approval processes of the U.S. Food and Drug Administration, or FDA, and comparable foreign authorities are lengthy, time consuming and inherently unpredictable. If we are not able to obtain, or if there are delays in obtaining, required additional regulatory approvals, we will not be able to commercialize our product candidates as expected, and our ability to generate revenue will be materially impaired. |
| ● | For our approved product, KORSUVA injection, we will be subject to ongoing obligations and continued regulatory review, which may result in significant additional expense. Additionally, our product candidates, if approved, could be subject to labeling and other restrictions and market withdrawal and we may be subject to penalties if we fail to comply with regulatory requirements or experience unanticipated problems with our products. |
3
| ● | Our products, including KORSUVA injection, may have undesirable side effects that may require them to be taken off the market, require them to include safety warnings or otherwise limit their sales. Further, our product candidates may have serious adverse events or undesirable side effects that may limit dosing in development, delay or prevent regulatory or marketing approval. |
| ● | If we experience continuous delays or difficulties in the enrollment of patients in clinical trials, our receipt of necessary regulatory approvals could be delayed or prevented. |
| ● | We have incurred significant losses from our inception, and we anticipate that we may incur losses in the foreseeable future. Our first commercial product was only recently approved, and we may never maintain profitability. |
| ● | We are dependent on third parties to decide to utilize KORSUVA injection and to make it readily available at the point of care throughout their dialysis centers or hospitals. |
| ● | We rely on third parties to perform many essential services for KORSUVA injection and may do so in the future for any products that we commercialize, including services related to warehousing and inventory control, distribution, customer service, accounts receivable management, cash collection and adverse event reporting. If these third parties fail to perform as expected or to comply with legal and regulatory requirements, our ability to commercialize KORSUVA injection or any other product candidate, will be significantly impacted and we may be subject to regulatory sanctions. |
| ● | We are dependent on our collaboration agreements for certain revenues, and if our commercial partners do not perform their obligations under such agreements, we could lose revenues. |
| ● | If the government or other third-party payers fail to provide coverage and adequate reimbursement and payment rates for KORSUVA injection or any of our other current or future product candidates, if any, or if providers choose to use therapies that are less expensive, our revenue and prospects for profitability will be limited. |
| ● | We may need to license certain intellectual property from third parties, and such licenses may not be available or may not be available on commercially reasonable terms. |
Industry and Market Data
We obtained the industry and market data in this Annual Report on Form 10-K from our own research as well as from industry and general publications, surveys and studies conducted by third parties. Industry and general publications, studies and surveys generally state that the information contained therein has been obtained from sources believed to be reliable. These third parties may, in the future, alter the manner in which they conduct surveys and studies regarding the markets in which we operate our business. As a result, you should carefully consider the inherent risks and uncertainties associated with the industry and market data contained in this Annual Report on Form 10-K, including those discussed in Part I Item 1A. “Risk Factors.”
Item 1. Business.
Overview
We are an early commercial-stage biopharmaceutical company leading a new treatment paradigm to improve the lives of patients suffering from pruritus. Our novel KORSUVA injection is the first and only FDA-approved treatment for moderate-to-severe pruritus associated with chronic kidney disease, or CKD, in adults undergoing hemodialysis. We are developing an Oral KORSUVA (difelikefalin) formulation and plan to initiate Phase 3 programs in the first quarter of 2022 for the treatment of pruritus in patients with atopic dermatitis, or AD, and non-dialysis-dependent chronic kidney disease, or NDD-CKD. Phase 2 trials of Oral KORSUVA (difelikefalin) are ongoing in primary biliary cholangitis, or PBC, and in NP patients with moderate-to-severe pruritus.
4
Our mission is to be the leader in the treatment of chronic pruritus and transform the way pruritus is treated to improve the quality of life for millions of people who suffer from pruritus. Our corporate strategy is focused on changing the standard of care and advancing the scientific understanding of pruritus. With this focus, we aim to be the leader in this treatment area across many diseases, where we believe there is significant, unresolved unmet need and significant value in meeting that need. Pruritus is a medical condition and yet few if any targeted treatment options are available for patients. In our estimation, based on available literature and market research, potentially millions of patients globally, could benefit from a therapy specifically targeting chronic pruritus. Many current therapies used in the pruritus treatment algorithm target another underlying disease condition. However, these therapies do not often sufficiently address pruritus, leaving patients with poor quality of life. Chronic pruritus manifests across primarily three key disease categories or subsets, and is a key effect in numerous (1) systemic diseases, (2) dermatological diseases, and (3) neurological diseases.
Our strategy seeks to leverage and maximize the highly novel mechanism of action of our lead asset, difelikefalin, to potentially treat pruritus across all three of these key disease categories. The first step in executing our strategy was the FDA approval of KORSUVA injection for the treatment of moderate-to-severe pruritus associated with CKD in adults undergoing hemodialysis. The approval sets in motion further plans for the impending U.S. commercial launch of KORSUVA injection, expected generation of revenue and regulatory submissions, potential future marketing approvals and commercialization in other countries.
The next step in our strategy is the ongoing late and mid-stage clinical development of an oral formulation of difelikefalin to potentially enable its use to expand across all three of the key disease categories with pruritus. A more convenient oral dosing could allow difelikefalin to reach more patients in more diseases, particularly more prevalent dermatologic, systemic, and neurologic conditions. Oral KORSUVA (difelikefalin) has the potential to significantly alter the treatment algorithm for chronic pruritus.
On August 23, 2021, our lead product, KORSUVA injection, was approved by the FDA for the treatment of moderate-to-severe pruritus associated with CKD in adults undergoing hemodialysis in the United States. We expect commercial launch of KORSUVA injection in April 2022 and associated revenues in the second quarter of 2022.
We have partnered with VFMCRP, a joint venture between Vifor Pharma Group and Fresenius Medical Care, and Vifor to commercialize KORSUVA injection in dialysis patients with CKD-aP in the U.S. under profit share agreements. We have partnered with VFMCRP to commercialize KORSUVA worldwide, excluding Japan (Maruishi/sub-licensee Kissei), and South Korea (CKDP). VFMCRP is a leading nephrology commercial organization with a significant presence in nephrology offices and dialysis centers. We are launching KORSUVA injection into a highly concentrated market. The dialysis market in the U.S. is dominated by two key providers, Fresenius and Davita, which combined control about 75% of the market. In addition, about 80% of the CKD hemodialysis patients are insured by Medicare.
Our U.S. commercial partner, Vifor Pharma Group, submitted the payment reimbursement application for Transition Drug Add-on Payment Adjustment, or TDAPA, and the Healthcare Common Procedure Coding System, or HCPCS, to the U.S. Center for Medicare & Medicaid Services, or CMS, in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years.
For the next phase of our strategy, we have built a pipeline around an oral formulation of difelikefalin, the active compound in KORSUVA injection. We are developing Oral KORSUVA (difelikefalin) in programs to create potential opportunities across all three disease categories with chronic pruritus. This platform of Oral KORSUVA (difelikefalin) programs is designed to significantly expand the addressable market and patient populations that might benefit from our compound. We have four clinical programs in disease areas with about 16 million potential patients: NDD-CKD associated pruritus, AD, chronic liver disease, or CLD, and NP.
Based on our completed Phase 2 trials and FDA End of Phase 2 meetings, in the first quarter of 2022, we plan to initiate two Phase 3 registrational programs of Oral KORSUVA (difelikefalin) for the treatment of pruritus, one in NDD-CKD and the other in AD.
5
In earlier-stage programs, we have a Phase 2 study ongoing for Oral KORSUVA (difelikefalin) in the treatment of pruritus associated with NP. NP is a common neurosensory condition and chronic pruritus is the key manifestation of NP. This condition has no FDA-approved treatments nor robust data to support the use of any single therapy. We currently anticipate a readout on this trial in the second quarter of 2022. We believe this program could provide insight on Oral KORSUVA’s (difelikefalin) potential in other chronic neuropathic pruritus conditions. In addition, we have an ongoing Phase 2 study of Oral KORSUVA (difelikefalin) for the treatment of PBC for which we currently anticipate a readout in the second half of 2022. This program could provide insight into whether Oral KORSUVA (difelikefalin) has utility in other chronic liver diseases.
We were incorporated and commenced operations in 2004, and our primary activities to date have been organizing and staffing our company, developing our lead product and product candidates, including conducting preclinical studies and clinical trials of difelikefalin-based product candidates and raising capital. To date, we have financed our operations primarily through sales of our equity and debt securities and payments from license agreements.
Recent Developments
COVID-19 Update
The extent of the impact of the ongoing COVID-19 pandemic on our business, operations and clinical development and regulatory timelines and plans remains uncertain, and will depend on certain developments, including the duration and the outbreak and spread of variants and its impact on our clinical trial enrollment, trial sites, partners, CROs, third-party manufacturers, and other third parties with whom we do business, as well as its impact on regulatory authorities and our key scientific and management personnel. The timing of our submission of our new drug application, or NDA, to the FDA for KORSUVA injection was not affected, as we submitted the NDA in December 2020. The COVID-19 pandemic, however, has affected, and may in the future affect, the initiation of certain trial sites and patient enrollment for our ongoing Phase 2 clinical trials of Oral KORSUVA (difelikefalin) for moderate-to-severe pruritus in patients with NP, and for the treatment of pruritus in patients with hepatic impairment due to PBC. While we currently do not expect any significant delays in our clinical development or commercial timelines, the ultimate impact of the evolving COVID-19 pandemic remains difficult to predict.
To the extent possible, we are conducting business as usual, with necessary or advisable modifications to employee travel and employee work locations. We are continuing to actively monitor the rapidly evolving situation related to COVID-19 and may take further actions that alter our operations, including those that may be required by federal, state or local authorities, or that we determine are in the best interests of our employees, partners and other third-parties with whom we do business. The extent to which the ongoing and evolving COVID-19 pandemic may affect our business, operations and clinical development and regulatory timelines and plans, including the resulting impact on our expenditures and capital needs, remains uncertain.
Vifor and VFMCRP Milestone Payments
In October 2021, after the expiration of the requisite waiting period under the Hart-Scott-Rodino Antitrust Improvement Act of 1976, or the HSR Act, we received a $50.0 million milestone payment from Vifor and issued 3,282,391 shares of our common stock in connection with U.S. regulatory approval of KORSUVA injection on August 23, 2021 (see Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations – Collaboration and License Agreements – Vifor (International) Ltd.).
Also in October 2021, we received a $15.0 million milestone payment from VFMCRP in connection with U.S. regulatory approval of KORSUVA injection on August 23, 2021 (see Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations – Collaboration and License Agreements – VFMCRP).
Christopher Posner Appointed as President and Chief Executive Officer
Christopher Posner was appointed as our President and Chief Executive Officer, or CEO, effective November 9, 2021. Mr. Posner joins us from LEO Pharma, Inc., the U.S. affiliate of LEO Pharma A/S, a global leader in medical
6
dermatology, where he was President and CEO. Mr. Posner succeeds Dr. Derek Chalmers, who transitioned to a Senior Advisor role to us.
Overview of Need in Chronic Pruritus
Pruritus, or itch, is defined as an unpleasant sensation that provokes the desire to scratch, which can range from a mild annoyance to an intractable, disabling condition. Chronic pruritus is a significant unmet need with few if any robustly efficacious or pruritus-targeting treatment options. Overall, about one in every eight people globally suffer from chronic pruritus. The condition is often under-reported by patients and often under-treated. The result is a significant and sometimes disabling impact on patients’ quality of life.
Chronic pruritus occurs in primarily three broad disease subsets: systemic diseases, dermatological diseases, and neurological diseases. Each disease category has numerous individual diseases with which chronic pruritus is associated or a key symptomatic feature of that condition.
Certain systemic diseases known to cause pruritus include endocrine and metabolic disease such as CKD and chronic liver disease like PBC, infectious disease, hematologic and lymphoproliferative diseases, visceral neoplasms and drug-induced pruritus.
Dermatological diseases known to cause pruritus include inflammatory dermatoses – such as AD, infectious dermatoses, autoimmune dermatoses, neoplasms, genodermatoses, and dermatoses of pregnancy.
Neurological diseases known to have pruritus include NP, brachioradial pruritus and post-herpetic neuralgia.
Each one of these categories and disease subsets areas has potential as an area of exploration for our lead product, difelikefalin. The unaddressed unmet need remains substantial. According to a study we conducted with IQVIA utilizing medical claims data from 2019, or the IQVIA study, approximately 23 million patients were diagnosed with diseases known to trigger chronic pruritus and received a prescription for an anti-pruritic agent such as corticosteroids, antihistamines, select antidepressants, counterirritants, bile acid sequestrants, rifampin, narcotic antagonists, and partial agonists, topical immunomodulators or gabapentin.
Role of Peripheral Kappa Opioid Receptor (KOR) Agonist in Pruritus
Recent advancements in the understanding of the biology of pruritus have led to the discovery of novel targets in the central nervous system, or CNS, and a unique pathway central to chronic pruritus. Pruritus, commonly referred to as itch, originates in the epidermis and dermal–epidermal junction and is transmitted by itch-selective sensory neuron C fibers, or pruriceptors. Some of these fibers are sensitive to histamine while others are not, and there is evidence for histamine-insensitive C fibers that are activated by numerous itch-inducing substances or pruritogens, many of which initiate signals through interaction with specific G-protein-coupled receptors. In addition, there is increasing evidence for the differential involvement of these systems in various forms of itch which may involve disease-specific pruritogens. As an example, chronic pruritus associated with kidney failure is thought to involve complex interactions among peripheral cells (T cells, mast cells, neutrophils, eosinophils, and keratinocytes) and histamine-insensitive nerve fibers, involving increased release of cytokines, proteases, and neuropeptides, interacting with multiple receptors that lead to exacerbation of itch.
These different peripheral cell types express kappa opioid receptors, or KORs, which can regulate the release of these pruritogenic substances, while the KORs on C fibers are thought to regulate their response to these pruritogens. Because KORs are expressed in peripheral tissues, there is a potential to modulate itch signals peripherally without impacting the central KORs. The itch-sensitive sensory nerve fibers transmit signals to the cell bodies in the dorsal root ganglia (that also have KORs), which send fibers to enter the spinal cord. Itch signals then ascend via the spinothalamic tract to multiple brain areas for sensory processing and interactions with cognitive and other systems. Additionally, the activation of kappa receptors via an agonist is thought to reduce itching by functionally counteracting increased mu opioid receptor activity which is suggested to be associated with some chronic forms of pruritus. Activation of the mu opioid receptor in the brain and in the peripheral nerve endings results in itching while non-selective mu opioid
7
antagonists can inhibit itching. KOR stimulation inhibits the effects of mu receptor activation both centrally and peripherally.
Our novel compound, difelikefalin, is a highly selective, predominantly peripherally acting KOR agonist. Its design includes specific characteristics that limit entry into the CNS. As a KOR agonist, difelikefalin’s mechanism of action turns off the itch sensation by acting on the peripheral neurons responsible for sensing pruritus. In other words, difelikefalin disrupts the itch sensation of chronic pruritus at the nerve level. In addition, difelikefalin acts on KORs expressed on a range of activated immune cells to subsequently block the release of pruritogenic cytokines. A central hypothesis driving our development work is that by acting on peripheral nerves that sense pruritus, difelikefalin may be able to address pruritus regardless of the underlying disease state.
Corporate Strategy
Our mission is to be the leader in the treatment of chronic pruritus and transform the way pruritus is treated to improve the quality of life for millions of people who suffer from pruritus. Our corporate strategy is focused on changing the standard of care and advancing the scientific understanding of pruritus. The strategy seeks to leverage and maximize the highly novel, first-in-class mechanism of action - peripherally acting KOR agonist - of our lead product, difelikefalin, to potentially treat pruritus across all three of these key disease categories. Our strategic priorities are to launch and maximize the commercial potential of KORSUVA injection and to develop Oral KORSUVA (difelikefalin) to expand across all categories of pruritus, thus changing how it is treated in practice. Key elements and priorities of the strategy include:
Optimize the commercial potential of KORSUVA injection in the U.S. and, if approved, throughout the rest of the world. In August 2021, the FDA approved KORSUVA injection as the first and only FDA-approved therapy for the treatment of moderate-to-severe pruritis associated with CKD in adults undergoing hemodialysis. It was approved under Breakthrough Therapy Designation. In December 2021, CMS granted TDAPA reimbursement status, effective April 1, 2022, for two years. Our license and collaboration agreements to commercialize KORSUVA injection, which include sales and marketing infrastructure support from our partners, are a key part of our strategic focus to maximize the potential of our product rapidly and efficiently. We expect KORSUVA injection will be available to patients for commercial use in the U.S. in April 2022 and associated revenues in the second quarter of 2022.
Advance the Oral KORSUVA (difelikefalin) platform by initiating Phase 3 programs in chronic pruritus associated with NDD-CKD and AD. Building upon the KORSUVA injection approval in CKD-aP in adults undergoing hemodialysis, we completed Phase 2 trials for Oral KORSUVA (difelikefalin) in both NDD-CKD and AD associated pruritus and we conducted End of Phase 2 meetings with the FDA in 2021. We will initiate Phase 3 clinical trials in pruritus associated with NDD-CKD and pruritus associated with AD in the first quarter of 2022, with the goal of gaining indications in both.
Expand the Clinical Utility of Oral KORSUVA (difelikefalin) by pursuing indications for the treatment of chronic pruritus in NP and CLD. We believe that Oral KORSUVA’s (difelikefalin) novel mechanism of action offers a portfolio in a product opportunity and has therapeutic potential in several other patient populations with neurologic-related pruritus and CLD-aP. We initiated a Phase 2 program in NP in January 2021 and expect to report top-line data in the second quarter of 2022. We also have a Phase 2 program underway for Oral KORSUVA (difelikefalin) for the treatment of pruritus in patients with hepatic impairment due to PBC. We expect to have top-line data in the second half of 2022.
8
Our current product and product candidate pipeline is summarized in the table below:
Program |
| Product Candidate |
| Primary Indication |
| Status |
| Commercialization Rights |
Pruritus |
| KORSUVA (difelikefalin) injection |
| Pruritus CKD - Hemodialysis |
| • FDA approved in August 2021 |
| VFMCRP/Vifor (United States); Maruishi (Japan); CKDP (South Korea); VFMCRP (Worldwide, other than United States, Japan and South Korea) |
| Oral KORSUVA (difelikefalin) |
| Pruritus Atopic Dermatitis (AD-aP) |
| • Phase 2 trial completed; top-line data reported |
| Cara (Worldwide, other than South Korea); CKDP (South Korea) | |
| Oral KORSUVA (difelikefalin) |
| Pruritus NDD-CKD |
| • Phase 2 trial completed; top-line data reported |
| Cara (Worldwide, other than Japan and South Korea); Maruishi (Japan); CKDP (South Korea) | |
| Oral KORSUVA (difelikefalin) |
| Pruritus CLD - Primary Biliary Cholangitis (PBC) |
| • Phase 2 efficacy trial ongoing |
| Cara (Worldwide, other than South Korea); CKDP (South Korea) | |
| Oral KORSUVA (difelikefalin) |
| Notalgia Paresthetica (NP) |
| • KOMFORT Phase 2 efficacy trial ongoing |
| Cara (Worldwide, other than South Korea); CKDP (South Korea) |
Difelikefalin – Our Lead Product
Our product candidate, difelikefalin, is a new chemical entity, which is designed to selectively stimulate kappa, rather than mu, and delta opioid receptors. Difelikefalin has been designed with specific chemical characteristics to restrict its entry into the CNS and further limit its mechanism of action to KORs in the peripheral nervous system and on immune cells. Activation of kappa receptors in the CNS is known to result in some undesirable effects, including dysphoria. Since difelikefalin modulates kappa receptor signals peripherally without any significant activation of opioid receptors in the CNS, it is generally not expected to produce the CNS-related side effects of mu opioid agonists (such as addiction and respiratory depression) or centrally-active kappa opioid agonists (such as dysphoria and hallucinations). Difelikefalin has been administered to more than 3,000 human subjects in Phase 1, Phase 2 and Phase 3 clinical trials as an I.V. infusion, bolus intravenous injection or oral capsule or tablet, and thus far has been observed to be generally well tolerated in multiple clinical trials.
Based on the non-clinical and clinical studies we have completed to date, we believe that KORSUVA injection and Oral KORSUVA (difelikefalin) for our other product candidates, if approved, would be attractive to both patients and physicians as a treatment for chronic pruritus across the spectrum of systemic, neurological, and dermatological variations of the disease.
KORSUVA Injection for Moderate-to-Severe Pruritus Associated with CKD in Adults Undergoing Hemodialysis
CKD is a clinical condition wherein progressive kidney damage leads to an impairment of kidney function over time. Primary risk factors culminating into CKD include diabetes, hypertension, cardiovascular disease, or hereditary renal disease. Early-stage disease is generally associated with few mild clinical manifestations; however, CKD can progress to kidney failure or end-stage renal disease, or ESRD, which is fatal without dialysis or transplantation. According to the National Kidney Foundation, ESRD is estimated to affect approximately 750,000 individuals per year in the U.S., of which approximately 500,000 patients undergo regular dialysis.
9
Chronic pruritus is one of the many comorbidities of CKD, characterized by a highly unpleasant and irritating sensation that triggers an urge to scratch the skin. CKD-aP adversely affects patient quality of life and can result in infections, sleep-deprivation, depression, and even increased risk of mortality.
CKD-aP’s intractable systemic itch has a high prevalence. According to Fresenius Medical Care, a world leading provider of products and medical care for dialysis patients, there were approximately 3.2 million patients globally undergoing dialysis in 2017. According to the Dialysis Outcomes and Practice Patterns Study published in December 2017 in the Clinical Journal of the American Society of Nephrologists, it is estimated that nearly 70% of these patients suffer from some form of CKD-aP with approximately 40% of these patients experiencing moderate to severe pruritus.
KORSUVA Injection Approved by the FDA in August 2021
KORSUVA injection was approved by the FDA on August 23, 2021 and is the first and only product approved by the FDA for the treatment of moderate-to-severe pruritus associated with CKD in adult patients undergoing hemodialysis. KORSUVA injection is not scheduled as a controlled substance. The clinical development program was the largest in CKD-aP patients undergoing hemodialysis with over 1,300 patients participating.
In June 2017, the FDA granted Breakthrough Therapy Designation to KORSUVA injection for the treatment of CKD-aP in hemodialysis patients. The KORSUVA injection NDA received Priority Review by the FDA, which is granted to therapies that, if approved, would offer significant improvements in the safety or effectiveness of the treatment, diagnosis, or prevention of serious conditions when compared to standard applications.
KORSUVA injection is the first and only FDA-approved product in the United States to treat CKD-aP in adults undergoing hemodialysis. There are no approved products in Europe to treat CKD-aP. Patients are generally managed with a multitude of products including corticosteroids, gabapentin, antihistamines, antidepressants and others with limited efficacy and tolerability. There is one product, nalfurafine (Remitch®) marketed by Toray Industries, approved to treat CKD-aP in Japan, but not approved in either the U.S. or Europe.
In October 2020, we entered into a license agreement with Vifor pursuant to which we granted Vifor an exclusive license solely in the United States to use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA injection for all therapeutic uses relating to the inhibition, prevention or treatment of itch associated with pruritus in hemodialysis and peritoneal dialysis patients in the United States.
Our U.S. commercial partner, Vifor Pharma Group, submitted the payment reimbursement application for TDAPA and HCPCS to CMS in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years. CMS expressed in its written communication to us and Vifor Pharma, a continuing interest in engaging with the companies regarding potential post-TDAPA support to ensure all beneficiaries with ESRD have access to innovative products such as KORSUVA injection.
Commercialization of KORSUVA injection in the U.S is planned for April 2022 with associated revenues in the second quarter of 2022.
Clinical Results
KORSUVA injection was approved by the FDA on August 23, 2021 and is the first and only product approved for the treatment of moderate-to-severe pruritus associated with CKD in adult patients undergoing hemodialysis.
It was approved based on the NDA filing that was supported by positive data from two pivotal Phase 3 trials – KALMTM-1, conducted in the U.S., and the global KALM-2 trial, as well as supportive data from an additional 32 clinical studies. KORSUVA injection was found to be generally well tolerated in the pivotal studies highlighted below.
In April 2020, we announced positive top-line results from our KALM-2 pivotal Phase 3 trial of KORSUVA injection in hemodialysis patients with moderate-to-severe CKD-aP. The trial met the primary and key secondary
10
endpoints after 12 weeks of treatment. The study met the primary efficacy endpoint with 54% of the patients receiving 0.5 mcg/kg of KORSUVA injection versus 42% of patients receiving placebo achieving at least a three-point improvement from baseline with respect to the weekly mean of the daily 24-hour worst itching intensity numeric rating scale, or NRS, Table of Contents 11 score at week 12 (p= 0.02). The study also met the key secondary endpoint with 41% of patients receiving KORSUVA injection achieving a four-point or greater improvement from baseline in the weekly mean of the daily 24-hour worst itching NRS score at week 12 versus 28% for patients receiving placebo (p= 0.01). In this trial, KORSUVA injection was generally well-tolerated with a safety profile consistent with that seen in KALM-1 and the KORSUVA clinical program in patients with CKD-aP.
Overall, the incidence of adverse effects, or AEs, and serious AEs were similar across both KORSUVA injection and placebo groups. The most common treatment emergent AEs reported in greater than 5% of patients were diarrhea (8.1% KORSUVA vs 5.5% placebo), falls (6.8% KORSUVA vs 5.1% placebo), vomiting (6.4% KORSUVA vs 5.9% placebo), nausea (6.4% KORSUVA vs 4.2% placebo) and dizziness (5.5% KORSUVA vs 5.1% placebo).
In May 2019, we announced positive results from the double blinded phase of our KALM-1 pivotal Phase 3 efficacy trial of KORSUVA injection for the treatment of CKD-aP in patients undergoing hemodialysis. The trial met the primary and all secondary endpoints after 12 weeks of treatment. The study met the primary efficacy endpoint with 51% of the patients receiving 0.5 mcg/kg of KORSUVA injection versus 28% of patients receiving placebo achieving at least a three-point improvement from baseline with respect to the weekly mean of the daily 24-hour worst itching intensity NRS score at week 12 (p= 0.000019). The study also met all secondary endpoints, including assessment of itch-related quality of life changes measured using self-assessment Skindex-10 (patients receiving KORSUVA experienced 43% improvement versus patients receiving placebo, p= 0.0004) and 5-D Itch scales (patients receiving KORSUVA experienced 35% improvement versus patients receiving placebo, p= 0.0009). In addition, 39% of patients receiving KORSUVA injection achieved a four-point or greater improvement from baseline in the weekly mean of the daily 24-hour worst itching NRS score at week 12 versus 18% for patients receiving placebo (p= 0.000032), another key secondary endpoint. In this trial, KORSUVA injection was generally well-tolerated with a safety profile consistent with that seen in earlier trials.
Overall, the incidence of AEs and serious AEs were similar across both KORSUVA injection and placebo groups. The most common treatment emergent AEs reported in greater than 5% of patients were diarrhea (9.5% KORSUVA vs 3.7% placebo), dizziness (6.9% KORSUVA vs 1.1% placebo), vomiting (5.3% KORSUVA vs 3.2% placebo) and nasopharyngitis (3.2% KORSUVA vs 5.3% placebo).
Update on KORSUVA injection outside the U.S.
Our partner, VFMCRP, submitted a Marketing Authorization Application, or MAA, to the European Medicines Agency, or EMA, in March 2021, which was subsequently accepted for review by the EMA. If approved by the EMA, KORSUVA injection would receive marketing authorization in all member states of the European Union, or EU, as well as in Iceland, Liechtenstein, and Norway. The EMA’s decision on the EU MAA is expected in the second quarter of 2022.
In addition, our partner in Japan, Maruishi, announced positive Phase 3 top-line data in January 2022. Maruishi and its sublicensee Kissei confirmed the primary endpoint was achieved in a Japanese Phase 3 clinical study (double-blind, placebo-controlled period) of difelikefalin injection for the treatment of pruritus in hemodialysis patients. In the Phase 3 study, 178 patients were administered difelikefalin or placebo for 6 weeks followed by an open-label extension period of difelikefalin administration for 52 weeks. The primary endpoint, change in itch NRS score, and the secondary endpoint, change in itching scores of Shiratori severity criteria, were significantly improved from baseline compared to the placebo group. Difelikefalin was well-tolerated.
VFMCRP has submitted a marketing application for KORSUVA injection via the Access Consortium (which also includes applications to Canada, Switzerland, Australia, and Singapore) in the second quarter of 2021. Decision on this application is expected in the second quarter of 2022.
11
Oral KORSUVA (difelikefalin) Programs
Oral KORSUVA (difelikefalin) for Treatment of Non-Dialysis-Dependent Chronic Kidney Disease (NDD-CKD) Associated Pruritus
CKD-aP (also known as uremic pruritus) is a frequent and wearisome symptom in patients with NDD-CKD (Stage I – V). We are initiating a Phase 3 program with Oral KORSUVA (difelikefalin) for the treatment of pruritus in NDD-CKD, specifically in patients diagnosed with Stage IV and V CKD. There are approximately 1.2 million patients diagnosed with Stage IV and Stage V CKD in the United States and approximately 300,000 of these patients suffer from moderate-to-severe pruritus.
There are no FDA-approved treatment options specifically for this indication in the U.S. or Europe. Patients are generally managed with a multitude of products including corticosteroids, gabapentin, antihistamines, antidepressants, and others with varying degrees of success. There is one product, nalfurafine (Remitch®) marketed by Toray Industries, approved to treat CKD-aP in Japan, but not approved in either the U.S. or Europe.
In December 2019, we announced top-line data from our Phase 2 trial of Oral KORSUVA (difelikefalin) for the treatment of pruritus in NDD–CKD patients diagnosed with Stage III – V CKD. The Phase 2, multicenter, randomized, double-blind, placebo-controlled 12-week trial was designed to evaluate the safety and efficacy of three tablet strengths (0.25 mg, 0.5 mg and 1 mg, once daily administration) of Oral KORSUVA (difelikefalin) versus placebo in approximately 240 stage III - V (moderate-to-severe) CKD patients with moderate-to-severe pruritus. The primary efficacy endpoint was the change from baseline in the weekly mean of the daily 24-hour worst itching NRS score at week 12 of the treatment period. Secondary endpoints include change from baseline in itch-related quality of life scores at the end of week 12, as assessed by the total Skindex-10 and 5-D itch scores, as well as the proportion of patients achieving an improvement from baseline ≥3 points with respect to the weekly mean of the daily 24-hour worst itching NRS score at week 12.
Patients treated with the 1 mg tablet strength of Oral KORSUVA (difelikefalin) achieved the primary endpoint of statistically significant reduction in weekly mean of the daily worst itching NRS scores vs. placebo after the 12-week treatment period (-4.4 difelikefalin vs. -3.3 placebo, p=0.018). The treatment was statistically significant after two weeks of treatment and sustained through the 12-week treatment period. Regarding secondary endpoints, the proportion of patients on 1 mg tablet strength achieving a 3 point or greater improvement from baseline in the weekly mean of the daily worst itching NRS score at week 12 was 72% vs. 58% for placebo but did not achieve statistical significance. Furthermore, patients on 1 mg tablet strength showed positive improvements vs. placebo in itch quality of life endpoints as measured using self-assessment Skindex-10 and 5-D Itch scales but did not achieve statistical significance.
Oral KORSUVA (difelikefalin) was generally well-tolerated with a safety profile consistent with that seen in earlier KORSUVA clinical trials. Overall, the incidence of treatment AEs were similar across difelikefalin and placebo groups. The most common AEs reported in >5% of patients in the 1 mg difelikefalin group vs. placebo were dizziness (7.5% difelikefalin vs. 0% placebo), fall (6% difelikefalin vs. 0% placebo), diarrhea (6% difelikefalin vs. 1.5% placebo) and constipation (6% difelikefalin vs. 3% placebo).
In April 2021, we held an End of Phase 2 Meeting with the FDA to discuss the results of the Phase 2 trial of Oral KORSUVA (difelikefalin) in NDD CKD-aP and the potential Phase 3 program. The FDA indicated the acceptability of Stage V pre-dialysis CKD patients as a viable patient population for a program. In November 2021, the FDA provided written guidance indicating the patient population can be expanded to include the group of Stage IV pre-dialysis patients with advanced CKD in a registration program consisting of two pivotal Phase 3 clinical trials.
We expect to initiate the Phase 3 NDD CKD-aP program in the first quarter of 2022.
12
Oral KORSUVA (difelikefalin) for Treatment of Moderate-to-Severe Pruritus Associated with Atopic Dermatitis (AD)
AD is a chronic, pruritic inflammatory dermatosis that affects up to 25% of children and 2% to 5% of adults. Chronic pruritus is one of the defining features of AD. The itch is so common in AD that AD is often described as the itch that rashes. The point prevalence of chronic pruritus ranges between 87% to 100% in AD. According to a study published in Allergy in 2018, the point prevalence in adults in the U.S. is 4.9%, or approximately 12 million adults. Both quality of life and psychosocial well-being are known to negatively correlate with itch severity. The associated psychosocial morbidity of this distressing symptom includes sleep disruption, depression, agitation, anxiety, altered eating habits, reduced self-esteem and difficulty concentrating.
Additionally, AD patients can be segmented into groups based on the severity of their skin lesions as well as the severity of their itch. In a study published in Annals of Allergy, Asthma Immunology in 2021, it was found that nearly 25% of AD patients had mild-to-moderate lesions but still had severe pruritus. This “itch dominant” AD phenotype has a significant unmet medical need as their skin lesions have been controlled, but their severe itch has persisted. Most times, these patients have tried available agents (i.e., topical therapies, including corticosteroids, antihistamines) to control pruritus related to their AD unsuccessfully resulting in a significant patient population that needs a new oral agent for pruritus relief.
In April 2021, we announced top-line data from our Phase 2 KARE clinical trial. The KARE Phase 2 trial was a randomized, double-blind, placebo-controlled study designed to evaluate the efficacy and safety of Oral KORSUVA (difelikefalin) for moderate-to-severe pruritus in 401 adult subjects with AD-aP. KARE enrolled 64% of patients characterized as mild-to-moderate (BSA<10%) and 36% falling into the moderate-to-severe category (BSA>10%). Subjects were randomized to three tablet strengths of Oral KORSUVA (difelikefalin): 0.25 mg, 0.5 mg and 1 mg taken twice daily (BID) versus placebo for 12 weeks followed by 4 weeks of an active extension phase. A prespecified interim conditional power assessment was conducted after approximately 50% of the originally targeted patient number completed the designated 12-week treatment period. Based on the Independent Data Monitoring Committee’s recommendation, the sample size for each of the 0.5 mg dose and placebo groups were increased, taking the total trial size up by 28%.
KARE’s primary efficacy endpoint was change from baseline in the weekly mean of the daily 24-hour Itch NRS score at week 12 of the treatment period for the intent to treat, or ITT, population. Although no dose group met this endpoint, a statistically significant improvement from baseline was evident as early as week 1 for the 1 mg dose group, which was sustained through 75% of the treatment period.
In a prespecified analysis, a statistically significant change in the primary efficacy endpoint was observed in the mild-to-moderate (BSA<10%) patient population (p=0.036, All doses vs placebo), which was evident at week 1 and sustained through the treatment period.
The key secondary endpoint for KARE was the assessment of the proportion of patients achieving an improvement from baseline of ≥4 points with respect to the weekly mean of the daily 24-hour Itch NRS score at week 12 (4-point Responder Analysis). No dose group met this endpoint for the ITT population.
Prespecified analysis by disease severity indicated a statistically significant improvement in the 4-point Responder Analysis in the mild-to-moderate (BSA<10%) patient population with 33% of difelikefalin-treated patients achieving a ≥4-point reduction in NRS at Week 12 versus 19% in the placebo group for the 0.5 mg dose (p=0.046). All doses performed similarly (0.25 mg, 0.5 mg, and 1 mg) versus placebo.
Oral KORSUVA (difelikefalin) was generally well-tolerated across all doses.
We conducted an End of Phase 2 Meeting with the FDA in the third quarter of 2021 and aim to initiate a Phase 3 program for the treatment of pruritus in AD patients in the first quarter of 2022.
13
Oral KORSUVA (difelikefalin) for Treatment of Moderate-to-Severe Pruritus Associated with Notalgia Paresthetica (NP)
NP is a common, neurosensory condition caused by alteration and damage to thoracic spinal nerves and is characterized by chronic pruritus in the upper back. It is estimated that chronic pruritus affects up to 13% of the United States population. NP falls within the subcategory of chronic neuropathic pruritus which comprises approximately 8% of all cases of chronic pruritus. According to the IQVIA study, an estimated 1 million patients were diagnosed by dermatologists with ICD10 codes commonly used for NP in the United States.
There are no FDA-approved treatments for NP. The management of NP is challenging and conventional treatments for pruritus, such as antihistamines and topical steroids, are largely ineffective.
In January 2021, we initiated a Phase 2 randomized, double-blind, placebo-controlled trial that is designed to evaluate the efficacy and safety of Oral KORSUVA (difelikefalin) for moderate-to-severe pruritus in approximately 120 adult subjects with NP. Subjects were randomized to receive Oral KORSUVA (difelikefalin) 2 mg twice daily versus placebo for eight weeks followed by a 4-week active extension period and follow-up visit approximately 14 days after the last dose of the study. The primary efficacy endpoint is the change from baseline in the weekly mean of the daily 24-hour worst itching NRS score at week 8 of the treatment period. Secondary endpoints include improvement in itch-related quality of life assessed by the change from baseline to Week 8 and a change from baseline in itch-related sleep disturbance subscale measured by the itch medical outcomes study at week 8.
We currently aim to have top-line data in the second quarter of 2022.
Oral KORSUVA (difelikefalin) for Treatment of Chronic Liver Disease-Associated Pruritus (CLD-aP)
Pruritus develops in association with chronic liver diseases including hepatitis, liver cirrhosis, and PBC. It is estimated that approximately 6 million patients were diagnosed with CLD in 2019 in the United States and approximately 3 million patients received a prescription for an anti-pruritic. There are no FDA-approved therapies for pruritus associated with CLD, including PBC. Current antipruritic therapies, primarily antihistamines and corticosteroids as well as other therapies tried off-label, are largely ineffective in treating the disease and/or can produce significant side effects.
We are currently evaluating Oral KORSUVA (difelikefalin) in PBC for which it has been estimated that 70% of patients experience pruritus to initially establish the proof-of-concept in CLD-aP.
In June 2019, we announced the initiation of a Phase 2 trial of Oral KORSUVA (difelikefalin) for the treatment of pruritus in patients with hepatic impairment due to PBC. The Phase 2 multicenter, randomized, double-blind, placebo-controlled 16-week trial is designed to evaluate the safety and efficacy of a 1 mg tablet of Oral KORSUVA (difelikefalin) taken twice daily versus placebo in approximately 60 patients with PBC and moderate-to-severe pruritus. The primary efficacy endpoint is the change from baseline in the weekly mean of the daily 24-hour worst itching NRS score at week 16 of the treatment period. Secondary endpoints include change from baseline in itch-related quality of life scores at the end of week 16 as assessed by the Skindex-10 and 5-D itch scales, as well as the assessment of proportion of patients achieving an improvement from baseline of ≥3 points with respect to the weekly mean of the daily 24-hour worst itching NRS score at week 16. We continue to screen patients in this ongoing Phase 2 trial and, primarily due to the ongoing effects of the COVID-19 pandemic on patient enrollment, we currently aim to have top-line data in the second half of 2022.
Intravenous Difelikefalin for Treatment of Acute Postoperative Pain (PONV)
We have also investigated difelikefalin for the treatment of pain in an acute care setting. Difelikefalin is designed to provide pain relief without stimulating mu opioid receptors and therefore potentially without mu opioid-related side effects, such as nausea, vomiting, respiratory depression and euphoria.
14
In June 2018, we reported positive top-line data from the adaptive Phase 2/3 post-operative pain trial of I.V. difelikefalin in patients undergoing abdominal surgeries. At the higher dose of 1 mcg/kg dose, I.V. difelikefalin demonstrated statistically significant reductions in pain intensity compared to placebo at all pre-specified post-operative assessment periods. Additionally, I.V. difelikefalin treatment resulted in statistically significant reductions in the incidence of post-operative nausea and vomiting over the 24-hour period post-surgery for both the lower and higher doses of 0.5 and 1 mcg/kg, respectively.
At this time, we have de-prioritized this program as part of our strategy to focus on pruritus.
Collaboration and License Agreements
Vifor (International) Ltd. (Vifor)
In October 2020, we entered into a license agreement, or the Vifor Agreement, with Vifor under which we granted Vifor an exclusive license solely in the United States to use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA (difelikefalin) injection for all therapeutic uses relating to the inhibition, prevention or treatment of itch associated with pruritus in hemodialysis and peritoneal dialysis patients in the United States. Under the Vifor Agreement, we retain all rights with respect to the clinical development of, and activities to gain regulatory approvals of, KORSUVA (difelikefalin) injection in the United States.
Under the terms of the Vifor Agreement, we received from Vifor an upfront payment of $100.0 million and an additional payment of $50.0 million for the purchase of an aggregate of 2,939,552 shares of our common stock at a price of $17.0094 per share, which represents a premium over a pre-determined average closing price of our common stock. The purchase of our common stock was governed by a separate stock purchase agreement, or the Vifor Stock Purchase Agreement.
After U.S. regulatory approval of KORSUVA injection in August 2021, we received an additional $50.0 million in October 2021 for the purchase of an aggregate of 3,282,391 shares of our common stock at a price of $15.23 per share, which represents a 20% premium to the 30-day trailing average price of our common stock. The purchase of our common stock was governed by the Vifor Stock Purchase Agreement. The excess of the stock purchase price over the cost of the purchased shares at the closing price of our common stock on the date of the achievement of the milestone of $5.0 million was included as license and milestone fees revenue for accounting purposes for the year ended December 31, 2021. In addition, pursuant to the Vifor Agreement, we are eligible to receive payments of up to $240.0 million upon the achievement of certain sales-based milestones (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
We retain the right to make and have made KORSUVA injection, on a non-exclusive basis, in the United States for commercial sale of KORSUVA injection for use in all therapeutic uses to prevent, inhibit or treat itch associated with pruritus in hemodialysis and peritoneal-dialysis patients anywhere in the world and for supply of KORSUVA injection to Vifor under the terms of a supply agreement, or the Vifor Supply Agreement, which was executed in September 2021. The supply price is our cost of goods sold, or COGS, as calculated under generally-accepted accounting principles in the United States, or GAAP, plus an agreed upon margin. The Vifor Supply Agreement will co-terminate with the Vifor Agreement.
The Vifor Agreement provides full commercialization rights in dialysis clinics to Vifor in the United States under a profit-sharing arrangement. Pursuant to the profit-sharing arrangement, we will generally be entitled to 60% of the net profits (as defined in the Vifor Agreement) from sales of KORSUVA injection in the United States (excluding sales to Fresenius Medical Center dialysis clinics, compensation for which is governed by the VFMCRP Agreement) and Vifor is entitled to 40% of such net profits, subject to potential temporary adjustment in future years based on certain conditions. Under the Vifor Agreement, in consideration of Vifor’s conduct of the marketing, promotion, selling and distribution of KORSUVA injection in the United States, we will pay a marketing and distribution fee to Vifor based on the level of annual net sales. This fee will be deducted from product sales in calculating the net profits that are subject to the profit-sharing arrangement under the Vifor Agreement.
15
The Vifor Agreement will continue in effect until its expiration upon the cessation of commercial sale of KORSUVA injection in the United States by Vifor and its affiliates and sublicensees, or until the earlier termination of the Vifor Agreement.
In connection with the Vifor Agreement, the parties entered into a separate stock purchase agreement, or the Vifor Purchase Agreement, governing the issuance of our common stock to Vifor. Pursuant to the Vifor Purchase Agreement, Vifor will not, and will not cause any direct or indirect affiliate to, during the period beginning on October 15, 2020 and ending at the close of business on October 15, 2022, or the Restricted Period, (i) offer, pledge, sell, contract to sell, sell any option or contract to purchase, purchase any option or contract to sell, grant any option, right or warrant to purchase, lend, or otherwise transfer or dispose of, directly or indirectly, any shares of our common stock or any securities convertible into or exercisable or exchangeable for our common stock (including without limitation, common stock or such other securities which may be deemed to be beneficially owned by Vifor in accordance with the rules and regulations of the SEC and securities which may be issued upon exercise of a stock option or warrant) owned by Vifor as of the date hereof or acquired prior to the end of the Restricted Period (collectively with the common stock, referred to as the Lock-Up Securities, except any such sale, option or contract by and between Vifor and one of its affiliates (including Vifor Pharma Group Ltd. or VFMCRP), (ii) enter into any hedging, swap or other agreement or transaction that transfers, in whole or in part, any of the economic consequences of ownership of the Lock-Up Securities, whether any such transaction described in clause (i) or (ii) above is to be settled by delivery of Lock-Up Securities, in cash or otherwise, (iii) make any demand for or exercise any right with respect to the registration of any Lock-Up Securities, or (iv) publicly disclose the intention to do any of the foregoing.
Under the Vifor Purchase Agreement, the parties also agreed that, in certain circumstances, upon the request of Vifor, the parties will enter into a registration rights agreement prior to the end of the Restricted Period that would provide Vifor (or its affiliate transferee) customary registration rights with respect to the shares of common stock issued pursuant to the stock purchase agreement following the expiration of the Restricted Period.
Vifor Fresenius Medical Care Renal Pharma Ltd. (VFMCRP)
In May 2018, we entered into a license agreement, or the VFMCRP Agreement, with VFMCRP, a joint venture between Vifor Pharma Group and Fresenius Medical Care, under which we granted VFMCRP a license to seek regulatory approval to commercialize, import, export, use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA (difelikefalin) injection for all therapeutic uses to prevent, inhibit or treat itch associated with pruritus in hemodialysis and peritoneal-dialysis patients worldwide (excluding the United States, Japan and South Korea). We retain full development and commercialization rights for KORSUVA injection for the treatment of CKD-aP in dialysis patients in the U.S. except in the dialysis clinics of Fresenius Medical Care North America, or FMCNA, where we and VFMCRP will promote KORSUVA injection under a profit-sharing arrangement.
Upon entry into the VFMCRP Agreement, VFMCRP made a non-refundable, non-creditable $50 million upfront payment to us and Vifor purchased 1,174,827 shares of our common stock for $20 million, at a premium for the price of $17.024 per share, which represented a premium over a pre-determined average closing price of our common stock. The purchase of our common stock was governed by a separate stock purchase agreement.
After U.S. regulatory approval of KORSUVA injection in August 2021, we received a $15.0 million regulatory milestone payment in October 2021, which was recorded as license and milestone fees revenue for the year ended December 31, 2021 (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
We are eligible to receive from VFMCRP additional regulatory and commercial milestone payments in the aggregate of up to $455.0 million, consisting of up to $15.0 million in regulatory milestones and up to $440.0 million in tiered commercial milestones, all of which are sales-related. We are also eligible to receive tiered double-digit royalty payments based on annual net sales, as defined, of KORSUVA (difelikefalin) injection in the licensed territories. In the United States, we and VFMCRP will promote KORSUVA (difelikefalin) injection in the dialysis clinics of FMCNA under a profit-sharing arrangement (subject to the terms and conditions of the VFMCRP Agreement) based on net FMCNA clinic sales recorded by us.
16
We retain the right to make and have made KORSUVA (difelikefalin) injection worldwide (excluding the United States, Japan and South Korea), or the Territory, for commercial sale by VFMCRP in or outside the Territory, and for supply of KORSUVA (difelikefalin) injection to VFMCRP under the terms of a supply agreement, or the VFMCRP Supply Agreement, which was executed in May 2020. The supply price is our COGS, as calculated under GAAP, plus an agreed upon margin. The VFMCRP Supply Agreement will co-terminate with the VFMCRP Agreement.
Maruishi Pharmaceutical Co., Ltd. (Maruishi)
In April 2013, we entered into a license agreement with Maruishi, or the Maruishi Agreement, under which we granted Maruishi an exclusive license to develop, manufacture and commercialize drug products containing difelikefalin in Japan in the acute pain and uremic pruritus fields. Maruishi has a right of first negotiation for any other indications for which we develop difelikefalin and, under certain conditions, Maruishi may substitute another pruritus indication for the uremic pruritus indication originally included in its license from us. Maruishi is required to use commercially reasonable efforts, at its expense, to develop, obtain regulatory approval for and commercialize difelikefalin in Japan. We are required to use commercially reasonable efforts, at our expense, to develop, obtain regulatory approval for and commercialize difelikefalin in the United States.
In January 2022, Maruishi and its sublicensee Kissei confirmed the primary endpoint was achieved in a Japanese Phase 3 clinical study (double-blind, placebo-controlled period) of difelikefalin injection for the treatment of pruritus in hemodialysis patients. In the Phase 3 study, 178 patients were administered difelikefalin or placebo for 6 weeks followed by an open-label extension period of difelikefalin administration for 52 weeks. The primary endpoint, change in itch NRS score, and the secondary endpoint, change in itching scores of Shiratori severity criteria, were significantly improved from baseline compared to the placebo group. Difelikefalin was well-tolerated.
Under the terms of the Maruishi Agreement, we received a non-refundable and non-creditable upfront license fee of $15.0 million and are eligible to receive up to an aggregate of $10.5 million in clinical development and regulatory milestones (before contractual foreign currency exchange adjustments). In January 2021, we met the milestone criteria, as set forth in the Maruishi Agreement, for Maruishi’s first initiation of a Phase 3 trial for uremic pruritus in Japan. As a result, we received the $2.0 million milestone payment ($1.9 million after contractual foreign currency exchange adjustments) in May 2021. As of December 31, 2021, we have received $4.5 million (before contractual foreign currency exchange adjustments) of clinical development and regulatory milestones from Maruishi. We are also eligible to receive a one-time sales milestone of one billion Yen when a certain sales level is attained. We also receive a mid-double-digit percentage of all non-royalty payments received by Maruishi from its sublicensees, if any. We are also eligible to receive tiered royalties based on net sales, if any, with minimum royalty rates in the low double digits and maximum royalty rates in the low twenties. Maruishi’s obligation to pay us royalties continues, on a product-by-product basis, until the expiration of the last-to-expire licensed patent covering such product or the later expiration of any market exclusivity period.
The Maruishi Agreement continues until terminated. Either we or Maruishi may terminate the Maruishi Agreement for the other party’s breach of the agreement or bankruptcy. Maruishi may terminate the agreement at any time at will. We may terminate the agreement as a whole if Maruishi challenges the licensed patent rights, and we may terminate the agreement with respect to any indication if Maruishi discontinues its development activities. In addition, in connection with the Maruishi Agreement, Maruishi made an $8.0 million equity investment in our company.
Chong Kun Dang Pharmaceutical Corporation (CKDP)
In April 2012, we entered into a license agreement with CKDP, or the CKDP Agreement, under which we granted CKDP an exclusive license to develop, manufacture and commercialize drug products containing difelikefalin in South Korea. CKDP is required to use commercially reasonable efforts, at its expense, to develop, obtain regulatory approval for and commercialize difelikefalin in South Korea. We are required to use commercially reasonable efforts, at our expense, to develop, obtain regulatory approval for and commercialize difelikefalin in the United States.
Under the terms of the CKDP Agreement, we received a non-refundable and non-creditable $0.6 million upfront payment and are eligible to receive up to an aggregate of $3.8 million in development and regulatory milestones (before
17
South Korean withholding taxes). During the year ended December 31, 2020, we received a milestone payment of $0.6 million (net of South Korean withholding tax) from CKDP, as set forth in the CKDP Agreement, for completion of a Phase 3 trial for uremic pruritus in the United States. As of December 31, 2021, we have received $2.3 million (before South Korean withholding tax) of development and regulatory milestones. We are also eligible to receive a mid-double-digit percentage of all non-royalty payments received by CKDP from its sublicensees, if any, and tiered royalties ranging from the high single digits to the high teens based on net sales, if any. CKDP’s obligation to pay us royalties continues, on a product-by-product basis, until the expiration of the last-to-expire licensed patent covering such product or the later expiration of any market exclusivity period.
The CKDP Agreement continues until CKDP no longer has any obligation to pay us royalties on any product. Either we or CKDP may terminate the CKDP Agreement for the other party’s breach of the CKDP Agreement or bankruptcy. CKDP may terminate the CKDP Agreement if any of the licensed patent rights is invalid, unenforceable, is narrowed in scope or is deemed unpatentable, except as a result of a challenge by CKDP, or a third party commercializes a product containing a compound identical to difelikefalin without infringing any of the licensed patent rights in South Korea. We may terminate the CKDP Agreement if CKDP challenges the licensed patent rights or if a third party in South Korea owns an issued patent that claims difelikefalin and CKDP’s sale of products would infringe that patent. In addition, in connection with the CKDP Agreement, CKDP made a $0.4 million equity investment in our company.
Manufacturing and License Agreements
Polypeptide Laboratories S.A. (PPL)
In July 2021, we entered into an Active Pharmaceutical Ingredient, or API, Commercial Supply Agreement with Polypeptide Laboratories S.A., or PPL, that defines each party’s responsibilities with respect to PPL’s manufacture and supply of API for the difelikefalin injection product candidate. Under the API Commercial Supply Agreement, PPL shall manufacture API at its facility for sale and supply to us, in the amounts as set forth in purchase orders to be provided by us. We will be required to purchase our requirements of API for each year of the term of the agreement, based on internal forecasts.
The API Commercial Supply Agreement will continue until the fifth anniversary of the approval by the FDA of the NDA for KORSUVA injection, unless the API Commercial Supply Agreement is earlier terminated, and will automatically be extended for successive five-year periods unless either party gives notice to the other party of its intention to terminate.
Enteris Biopharma, Inc. (Enteris)
In August 2019, we entered into a Non-Exclusive License Agreement, or the Enteris License Agreement, with Enteris. Pursuant to the Enteris License Agreement, Enteris granted to us a non-exclusive, royalty-bearing license, including the right to grant sublicenses, under certain proprietary technology and patent rights related to or covering formulations for oral delivery of peptide active pharmaceutical ingredients with functional excipients to enhance permeability and/or solubility, known as Enteris’s Peptelligence® technology, to develop, manufacture and commercialize products using such technology worldwide, excluding Japan and South Korea.
As consideration for the licensed rights under the Enteris License Agreement, we paid an upfront fee equal to $8.0 million, consisting of $4.0 million in cash and $4.0 million in shares of our common stock pursuant to the Enteris Purchase Agreement described below. As a result, we recognized $8.0 million of R&D expense related to the Enteris License Agreement during the year ended December 31, 2019.
We are also obligated, pursuant to the Enteris License Agreement, to pay Enteris (1) milestone payments upon the achievement of certain development, regulatory and commercial milestones and (2) low-single digit royalty percentages on net sales of licensed products, subject to reductions in specified circumstances. Until the second anniversary of the entry into the Enteris License Agreement, we had the right, but not the obligation, to terminate our obligation to pay any royalties under the Enteris License Agreement in exchange for a lump sum payment in cash, or the Royalty Buyout. We did not exercise our Royalty Buyout right and such right expired in August 2021. During the years ended December 31,
18
2021 and 2020, we paid $15.0 million and $5.0 million, respectively, to Enteris for milestones earned in relation to the Enteris License Agreement, which were recorded in R&D expense for the respective periods.
The Enteris License Agreement will expire on a country-by-country, licensed product-by-licensed product basis upon the later of (1) the expiration (or invalidation) of all valid claims in licensed patent rights that cover such product in such country, (2) the end of the calendar quarter in which generic competition (as defined in the Enteris License Agreement) occurs for such product in such country and (3) ten years from the first commercial sale of such product.
Either party may terminate the Enteris License Agreement upon written notice if the other party has failed to remedy a material breach within 60 days (or 30 days in the case of a material breach of a payment obligation). Enteris may terminate the Enteris License Agreement upon 30 days’ written notice to us if we or any of our affiliates formally challenge the validity of any licensed patent rights or assists a third party in doing so. We may terminate the Enteris License Agreement for any reason or no reason (a) prior to receipt of first regulatory approval for a licensed product in the United States for any indication upon 30 days’ prior written notice to Enteris or (b) on or after receipt of first regulatory approval for a licensed product in the United States for any indication upon 60 days’ prior written notice to Enteris.
In August 2019, in connection with the Enteris License Agreement, we entered into the Enteris Purchase Agreement with Enteris and its affiliate, EBP Holdco LLC, collectively referred to as Purchaser, pursuant to which we issued and sold to Purchaser 170,793 shares of our common stock in a private placement. Such shares were issued in satisfaction of the $4.0 million portion of the upfront fee payable in shares of our common stock pursuant to the Enteris License Agreement and for no additional consideration, based on a purchase price of $23.42 per share, which was equal to the 30-day volume weighted average price of our common stock on August 20, 2019. Pursuant to the Enteris Purchase Agreement, we effected the registration and sale of the shares issued and sold to Purchaser thereunder in accordance with the applicable requirements of the Securities Act of 1933, as amended, or the Securities Act, which included the filing of a registration statement with the SEC on September 9, 2019. In addition, the Purchase Agreement includes customary representations, warranties and covenants by us.
Patheon UK Limited (Patheon)
In July 2019, we entered into a Master Manufacturing Services Agreement, or MSA, with Patheon UK Limited, or Patheon. The MSA governs the general terms under which Patheon, or one of its affiliates, will provide non-exclusive manufacturing services to us for the drug products specified by us from time to time. Pursuant to the MSA, we have agreed to order from Patheon at least a certain percentage of our commercial requirements for a product under a related Product Agreement. Each Product Agreement that we may enter into from time to time will be governed by the terms of the MSA, unless expressly modified in such Product Agreement.
The MSA has an initial term ending December 31, 2023, and will automatically renew after the initial term for successive terms of two years each if there is a Product Agreement in effect, unless either party gives notice of its intention to terminate the MSA at least 18 months prior to the end of the then current term.
Either party may terminate the MSA or a Product Agreement upon written notice if the other party (1) has failed to remedy a material breach within a specified time or (2) is declared insolvent or bankrupt, voluntarily files a petition of bankruptcy or assigns such agreement for the benefit of creditors. We may terminate a Product Agreement (a) upon 90 days’ prior written notice if any governmental agency takes any action that prevents us from selling the relevant product in the relevant territory, (b) upon six months’ prior written notice if we do not intend to order manufacturing services due to a product’s discontinuance in the market, or (c) upon 90 days’ prior written notice if we determine that the manufacture or supply of a product likely infringes third-party rights. Patheon may terminate the MSA or a Product Agreement (i) upon six months’ prior written notice if we assign such agreement to an assignee that is unacceptable to Patheon for certain reasons, or (ii) upon 30 days’ prior written notice if, after the first year of commercial sales, we forecast zero volume for 12 months.
The MSA contains, among other provisions, customary representations and warranties by the parties, a grant to Patheon of certain limited license rights to our intellectual property in connection with Patheon’s performance of the
19
services under the MSA, certain indemnification rights in favor of both parties, limitations of liability and customary confidentiality provisions.
Also in July 2019, we entered into two related Product Agreements under the MSA, one with each of Patheon and Patheon Manufacturing Services LLC, or Patheon Greenville, to govern the terms and conditions of the manufacture of commercial supplies of difelikefalin injection, our lead product candidate. Pursuant to the Product Agreements, Patheon and Patheon Greenville will manufacture commercial supplies of difelikefalin injection at the Monza, Italy and Greenville, North Carolina manufacturing sites, respectively, from API supplied by us. Patheon and Patheon Greenville will be responsible for supplying the other required raw materials and packaging components, and will also provide supportive manufacturing services such as quality control testing for raw materials, packaging components and finished product.
Sales and Marketing
In executing our strategy, our goal is to commercialize KORSUVA injection in the dialysis setting by partnering with out-licensing agreements, and to maintain significant control over the development process and commercial execution for the oral formulation of difelikefalin, if approved.
We have executed out-licensing agreements on KORSUVA injection in the dialysis setting in the United States and the rest of the world. Per the terms of the associated licensing agreement, Vifor Pharma will commercialize KORSUVA injection, and we will not be incurring costs for commercializing in the United States as we will be relying on sales and marketing infrastructure support from our partner.
For Oral KORSUVA (difelikefalin), we plan to develop and commercialize our drug candidate in pruritus indications, such as CKD-aP, AD, and potentially others, on our own in the United States, while exploring partnerships for development and commercialization in geographical territories outside the United States.
In 2015, we commissioned a qualitative market research study of nephrologists to evaluate the commercial potential of KORSUVA injection for CKD-aP. The study suggests KORSUVA injection would be well received by nephrologists, once approved. The key findings from the study were:
| ● | There is a clear unmet need to manage CKD-aP among dialysis patients. |
| ● | Currently, there are no effective options for severe CKD-aP. |
| ● | KORSUVA injection demonstrates strong efficacy for CKD-aP. |
| ● | KORSUVA injection can easily be incorporated into dialysis sessions. |
As a result, we believe that KORSUVA injection is well positioned to address the unmet needs for hemodialysis patients suffering from CKD-aP.
Intellectual Property
We strive to protect the proprietary technologies that we believe are important to our business, including seeking and maintaining patent protection intended to cover the composition of matter of our product candidates, their methods of use, related technology and other inventions that are important to our business. As more fully described below, patent applications have been filed covering compositions and novel formulations of these compositions, as well as methods of using difelikefalin. We own the patent portfolio of eighteen issued U.S. patents covering KOR agonists, sixteen of which cover composition of matter of difelikefalin and its uses; six of these include composition of matter claims directed to difelikefalin, and ten patents include claims to its uses. All of these U.S. patents covering difelikefalin and its uses are expected to expire no earlier than November 12, 2027. Additionally, three U.S. patents have been granted with claims to difelikefalin-like dimer compounds and their uses. We have filed patent applications in the U.S. and internationally
20
claiming novel oral formulations of difelikefalin. One U.S. patent with claims to oral formulations of difelikefalin has been granted and is expected to expire no earlier than September 13, 2039. Related U.S. and foreign applications, if granted, would also be expected to expire no earlier than September 13, 2039. We have also filed U.S. and foreign patent applications for additional formulations of difelikefalin, which if granted, would be expected to expire no earlier than March 18, 2040. We also rely on trade secrets and careful monitoring of our proprietary information to protect aspects of our business that are not amenable to, or that we do not consider appropriate for, patent protection.
Our success will depend significantly on our ability to obtain and maintain patent and other proprietary protection for commercially important technology, inventions and know-how related to our business, defend and enforce our patents, maintain our licenses to use intellectual property owned by third parties, preserve the confidentiality of our trade secrets and operate without infringing valid and enforceable patents and other proprietary rights of third parties. We also rely on know-how, and continuing technological innovation to develop, strengthen, and maintain our proprietary position in the field of peripheral analgesia and treatment of pruritus.
A third party may hold intellectual property, including patent rights, which are important or necessary to the development of our products. It may be necessary for us to use the patented or proprietary technology of third parties to commercialize our products, in which case we would be required to obtain a license from these third parties on commercially reasonable terms, or our business could be harmed, possibly materially. If we were not able to obtain a license or were not able to obtain a license on commercially reasonable terms, our business could be harmed, possibly materially.
We plan to continue to expand our intellectual property estate by filing patent applications directed to novel peripheral analgesics, novel formulations and novel uses of our proprietary compounds. We anticipate seeking patent protection in the United States and internationally for the chemistries and processes for manufacturing these compounds and novel formulations and uses of these compounds in a variety of therapies.
The patent positions of biopharmaceutical companies like us are generally uncertain and involve complex legal, scientific and factual questions. In addition, the coverage claimed in a patent application can be significantly reduced before the patent is issued, and the patent’s scope can be modified after issuance by later judicial decisions. Consequently, we do not know whether any of our product candidates will be adequately protectable or remain protected by enforceable patents. We cannot predict whether the patent applications we are currently pursuing will issue as patents in any particular jurisdiction or whether the claims of any issued patents will provide sufficient proprietary protection from competitors. Any patents that we hold may be challenged, circumvented or invalidated by third parties.
Because patent applications in the United States and certain other jurisdictions are maintained in secrecy for up to 18 months, and since publication of discoveries in the scientific or patent literature often lags behind actual discoveries, we cannot be certain of our entitlement to the inventions covered by pending patent applications. Moreover, although unlikely, we may have to participate in interference proceedings declared by the United States Patent and Trademark Office, or USPTO, to determine priority of invention, or in post-grant challenge proceedings in the USPTO, or a foreign patent office such as oppositions, inter-partes review, post grant review, or a derivation proceeding, that challenge our entitlement to an invention or the patentability of one or more claims in our patent applications or issued patents. Such proceedings could result in substantial cost, even if the eventual outcome is favorable to us.
The patent portfolios for our most advanced programs are summarized below.
Difelikefalin
Our synthetic peptide amide kappa opioid agonist patent portfolio is wholly owned by us. The portfolio includes eighteen issued U.S. patents (U.S. Patent Nos. 7,402,564; 7,713,937; 7,727,963; 7,842,662; 8,217,007; 8,236,766; 8,486,894; 8,536,131; 8,906,859; 8,951,970; 9,321,810; 9,334,305; 9,359,399; 10,017,536; 10,138,270; 10,793,596; 10,913,769 and 11,033,629) with claims to compositions of a wide range of synthetic peptide amide kappa opioid agonists, including difelikefalin and related molecules, as well as methods of using these compounds. These patents claiming difelikefalin compositions are due to expire November 12, 2027.
21
We have listed twelve of the patents claiming difelikefalin acetate and/or its uses in the Orange Book, a listing of patents relating to approved drug products maintained by the FDA. Difelikefalin acetate has been awarded a five-year exclusivity from the approval date, i.e. until August 23, 2026, prohibiting the FDA from accepting an application for approval of a difelikefalin product from a generic manufacturer until after the exclusivity period expires. In addition, we have also submitted an application for a patent term extension of one of our difelikefalin U.S. patents, which if granted for the full five-year extension requested, would extend the patent term to November 12, 2032.
Foreign applications relating to difelikefalin and related molecules, as well as methods of using these compounds, were filed in more than 40 foreign countries. National patents have been granted in 27 European countries, as well as in Australia, Brazil, Canada, China, Hong Kong, India, Israel, Japan, Malaysia, Mexico, New Zealand, Russian Federation, Singapore, South Africa and South Korea. These granted foreign patents with claims to difelikefalin are due expire no earlier than November 12, 2027.
Other Cara Patents and Patent Applications
We also own several other U.S. patents including U.S. Patent Nos. 7,741,350; 7,960,376; 7,960,377; and 8,211,926 with claims to other cannabinoid compounds and U.S. Patent No. 8,217,000 with claims to regulation of prolactin in mammals including humans.
The term of individual patents depends upon the legal term of the patents in the countries in which they are obtained. In most countries in which we file, the patent term is 20 years from the earliest date of filing a PCT application or a non-provisional patent application. The term of a patent in the United States can be adjusted and extended due to the failure of the USPTO following certain statutory and regulation deadlines for progressing prosecution and issuing a patent.
In the United States, the patent term of a patent that covers an FDA-approved drug may also be eligible for patent term extension, which permits patent term restoration as compensation for a portion of the patent term lost during the FDA regulatory review process. The Hatch-Waxman Act permits a patent term extension of up to five years beyond the expiration of the patent. The length of the patent term extension is related to the length of time the drug is under regulatory review. Patent extension cannot extend the remaining term of a patent beyond a total of 14 years from the date of product approval and only one patent applicable to an approved drug may be extended. Similar provisions are available in Europe and other non-United States jurisdictions to extend the term of a patent that covers an approved drug. In the future, if and when our pharmaceutical products receive FDA approval, we expect to apply for patent term extensions on patents covering those products. Although we intend to seek patent term extensions to any of our issued patents in any jurisdiction where these are available there is no guarantee that the applicable authorities, including the FDA in the United States, will agree with our assessment of whether such extensions should be granted, and even if granted, the length of such extensions.
We also rely on trade secret protection for our confidential and proprietary information. Although we take steps to protect our proprietary information and trade secrets, including through contractual means with our employees and consultants, third parties may independently develop substantially equivalent proprietary information and techniques or otherwise gain access to our trade secrets or disclose our technology. Thus, we may not be able to meaningfully protect our trade secrets. It is our policy to require our employees, consultants, outside scientific collaborators, sponsored researchers and other advisors to execute confidentiality agreements upon the commencement of employment or consulting relationships with us. These agreements provide that all confidential information concerning our business or financial affairs developed or made known to the individual during the course of the individual’s relationship with us is to be kept confidential and not disclosed to third parties except in specific circumstances. In the case of employees, the agreements provide that all inventions conceived by the individual, and which are related to our current or planned business or research and development, or R&D, or made during normal working hours, on our premises or using our equipment or proprietary information, are our exclusive property.
22
Competition
The biotechnology and pharmaceutical industries are characterized by rapidly advancing technologies, intense competition and a strong emphasis on proprietary products. While we believe that our technology, knowledge, experience and scientific resources provide us with competitive advantages, we face potential competition from many different sources, including large pharmaceutical and biotechnology companies, specialty pharmaceutical and generic drug companies, and medical technology companies. Any product candidates that we successfully develop and commercialize will compete with existing therapies and new therapies that may become available in the future.
There are a large number of companies developing or marketing therapies for the indications that we are pursuing. Many of our competitors, including many of the organizations named below, have substantially greater financial, technical and human resources than we do and significantly greater experience in the development of product candidates, obtaining FDA and other regulatory approvals of products and the commercialization of those products. Mergers and acquisitions in the pharmaceutical and biotechnology industries may result in even more resources being concentrated among a smaller number of competitors. Small or early-stage companies may also prove to be significant competitors, particularly through collaborative arrangements with large and established companies. We also compete with these companies in recruiting and retaining qualified scientific personnel and establishing clinical trial sites and patient registration for clinical trials.
We believe the key competitive factors that will affect the development and commercial success of our product candidates, if approved for marketing, are likely to be their safety, efficacy and tolerability profile, reliability, convenience of dosing, price and reimbursement from government and third-party payers. Our commercial opportunity could be reduced or eliminated if our competitors develop and commercialize products that are safer, more effective, have fewer or less severe side effects, are more convenient or are less expensive than any products that we may develop. Our competitors also may obtain FDA or other regulatory approval for their products more rapidly than we may obtain approval for ours, which could result in our competitors establishing a strong market position before we are able to enter the market. In addition, our ability to compete may be affected in many cases by insurers or other third-party payers seeking to encourage the use of generic products. Generic products that broadly address these indications are currently on the market for the indications that we are pursuing, and additional products are expected to become available on a generic basis over the coming years. If our product candidates achieve marketing approval, we expect that they will be priced at a significant premium over competitive generic products.
If our product candidates are approved for the indications for which we are currently undertaking clinical trials, they will compete with the therapies and currently marketed drugs discussed below:
KORSUVA Injection - Uremic Pruritus or CKD-aP. KORSUVA injection was approved on August 23, 2021 for the management of CKD-aP in adult hemodialysis patients. Currently, there are no approved products for management of CKD-aP in the United States. However, there are many products that are used to help manage CKD-aP. The most common of these agents are anti-itch creams and emollients as well as oral or injectable antihistamines. All of these products have limited degrees of efficacy and are available generically. Additionally, patients may try several other agents such as gabapentin or naltrexone, generally with limited success or therapies such as UVB light therapy with limited availability.
Because of the substantial unmet need for products that are safe and effective in CKD-aP, there are other companies that either were in the past or are currently involved in the discovery, development, and/or marketing of such products for CKD-aP or related conditions. Some of such product candidates or products include nemolizumab from Galderma, nalbuphine from Trevi Therapeutics and Remitch® or nalfurafine from Toray Industries.
Oral KORSUVA (difelikefalin) – Chronic Kidney Disease-Associated Pruritus (CKD-aP) and Chronic Liver Disease-Associated Pruritus (CLD-aP). We are developing Oral KORSUVA (difelikefalin) for the management of moderate-to-severe chronic pruritus conditions like CKD-aP or CLD-aP. There are currently no products approved in the United States for CKD-aP or CLD-aP. The market for the management of moderate-to-severe chronic pruritus is highly fragmented and includes numerous generic products, including oral formulations of corticosteroids and antihistamines. The most common corticosteroids and antihistamines are available generically. Because of the size and untapped
23
potential of the chronic pruritus market and the substantial unmet need for products that are safe and effective, there are other companies involved in the discovery, development, and/or marketing of new products for pruritus.
Oral KORSUVA (difelikefalin) – Atopic Dermatitis (AD)-Associated Pruritus. We are developing Oral KORSUVA (difelikefalin) for the management of moderate-to-severe chronic pruritus associated with AD. There are currently several products specifically approved in the United States to treat AD and the itching associated with it: Dupixent (dupilumab), Eucrisa (crisaborole), Opzelura (ruxolitinib), Adbry (tralokinumab-ldrm), Rinvoq (upadacitinib) and Cibinqo (abrocitinib). Additionally, the market for the management of mild-to-moderate and moderate-to-severe AD includes numerous generic products, including topical and oral formulations of corticosteroids and antihistamines. Because of the size and untapped potential of the AD market, there are other companies involved in the discovery, development, and/or marketing of new products for pruritus. Multiple companies are studying IL-13 inhibitors (e.g. lebrikizumab), IL-31 inhibitors (e.g. nemolizumab), JAK inhibitors (e.g. baricitinib) and OX40 inhibitors for treatment of AD.
Manufacturing
We do not have any manufacturing facilities. We currently rely, and expect to continue to rely, on third parties for the manufacture of our product candidates for preclinical and clinical testing, as well as for commercial manufacture for KORSUVA injection and if our product candidates receive marketing approval. We have negotiated long-term commitments with at least one primary supplier for our primary manufacturing and distribution functions. We have entered into a commercial manufacturing agreement with Patheon for KORSUVA injection, a commercial supply agreement with PPL to produce API, and a commercial packaging agreement with PCI Pharma Services.
All of our product candidates are either small peptides or organic small molecules and are manufactured in reliable and reproducible synthetic processes from readily available starting materials. The chemistry is amenable to scale up and does not require any special equipment or technology in the manufacturing process. We expect to continue to develop product candidates that can be produced cost-effectively at contract manufacturing facilities.
Government Regulation and Product Approval
Government authorities in the United States, at the federal, state and local level, and in other countries extensively regulate, among other things, the research, development, testing, manufacture, packaging, storage, recordkeeping, labeling, advertising, promotion, distribution, marketing, import and export of pharmaceutical products such as KORSUVA injection. The processes for obtaining regulatory approvals in the United States and in foreign countries, along with subsequent compliance with applicable statutes and regulations, require the expenditure of substantial time and financial resources.
FDA Regulation
In the United States, the FDA regulates drugs under the Federal Food, Drug, and Cosmetic Act, or FDCA, and its implementing regulations. The process of obtaining regulatory approvals and the subsequent compliance with appropriate federal, state, local and foreign statutes and regulations requires the expenditure of substantial time and financial resources. Failure to comply with the applicable United States requirements at any time during the product development process, approval process or after approval, may subject an applicant to a variety of administrative or judicial sanctions, such as the FDA’s refusal to approve pending NDAs, withdrawal of an approval, imposition of a clinical hold, issuance of warning or untitled letters, product recalls, product seizures, total or partial suspension of production or distribution, injunctions, fines, refusals of government contracts, restitution, disgorgement or civil or criminal penalties.
The process required by the FDA before a drug may be marketed in the United States generally involves the following:
| ● | completion of preclinical laboratory tests, animal studies and formulation studies in compliance with the FDA’s good laboratory practice, or GLP, regulations; |
24
| ● | submission to the FDA of an IND which must become effective before human clinical trials may begin; |
| ● | approval by an independent institutional review board, or IRB, at each clinical site before each trial may be initiated; |
| ● | performance of human clinical trials, including adequate and well-controlled clinical trials, in accordance with good clinical practices, or cGCP, to establish the safety and efficacy of the proposed drug product for each indication; |
| ● | submission to the FDA of an NDA; |
| ● | satisfactory completion of an FDA advisory committee review, if applicable; |
| ● | satisfactory completion of an FDA inspection of the manufacturing facility or facilities at which the product is produced to assess compliance with current good manufacturing practices, or cGMP, and to assure that the facilities, methods and controls are adequate to preserve the drug’s identity, strength, quality and purity, as well as satisfactory completion of an FDA inspection of selected clinical sites to determine cGCP compliance; and |
| ● | FDA review and approval of the NDA. |
Preclinical Studies. Preclinical studies include laboratory evaluation of drug substance chemistry, toxicity and drug product formulation, as well as animal studies to assess potential safety and efficacy. An IND sponsor must submit the results of the preclinical tests, together with manufacturing information, analytical data and any available clinical data or literature, among other things, to the FDA as part of an IND. Manufacture of drug substance, drug product and the labeling and distribution of clinical supplies must all comply with cGMP standards. Some preclinical testing may continue even after the IND is submitted. An IND automatically becomes effective 30 days after receipt by the FDA, unless before that time the FDA raises concerns or questions related to one or more proposed clinical trials and places the trial on a clinical hold. In such a case, the IND sponsor and the FDA must resolve any outstanding concerns before the clinical trial can begin. As a result, submission of an IND may not result in the FDA allowing clinical trials to commence.
Clinical Trials. Clinical trials involve the administration of the investigational new drug to human subjects under the supervision of qualified investigators in accordance with cGCP requirements, which include the requirement that all research subjects provide their informed consent in writing for their participation in any clinical trial. Clinical trials are conducted under protocols detailing, among other things, the objectives of the trial, the parameters to be used in monitoring safety and the effectiveness criteria to be evaluated. A protocol for each clinical trial and any subsequent protocol amendments must be submitted to the FDA as part of the IND. In addition, an IRB at each institution participating in the clinical trial must review and approve the plan for any clinical trial before it commences at that institution, and the IRB must continue to oversee the clinical trial while it is being conducted. Information about certain clinical trials must be submitted within specific timeframes to the National Institutes of Health, or NIH, for public dissemination on their ClinicalTrials.gov website.
Human clinical trials are typically conducted in three sequential phases, which may overlap or be combined. In Phase 1, the drug is initially introduced into healthy human subjects or patients with the target disease or condition and tested for safety, dosage tolerance, absorption, metabolism, distribution, excretion and, if possible, to gain an initial indication of its effectiveness. In Phase 2, the drug typically is administered to a limited patient population to identify possible adverse effects and safety risks, to preliminarily evaluate the efficacy of the product for specific targeted diseases and to determine dosage tolerance and optimal dosage. In Phase 3, the drug is administered to an expanded patient population, generally at geographically dispersed clinical trial sites, in well-controlled clinical trials to generate enough data to statistically evaluate the efficacy and safety of the product for approval, to establish the overall risk-benefit profile of the product and to provide adequate information for the labeling of the product.
25
Progress reports detailing the results of the clinical trials must be submitted at least annually to the FDA and more frequently if serious adverse events occur. Phase 1, Phase 2 and Phase 3 clinical trials may not be completed successfully within any specified period, or at all. Furthermore, the FDA or the sponsor may suspend or terminate a clinical trial at any time on various grounds, including a finding that the research subjects are being exposed to an unacceptable health risk. Similarly, an IRB can suspend or terminate approval of a clinical trial at its institution if the clinical trial is not being conducted in accordance with the IRB’s requirements or if the drug has been associated with unexpected serious harm to patients.
Marketing Approval. Assuming successful completion of the required clinical testing, the results of the preclinical and clinical studies, together with detailed information relating to the product’s chemistry, manufacture, controls and proposed labeling, among other things, are submitted to the FDA as part of an NDA requesting approval to market the product for one or more indications. In most cases, the submission of an NDA is subject to a substantial application user fee. Under the Prescription Drug User Fee Act, or PDUFA, guidelines that are currently in effect, the FDA has agreed to certain performance goals regarding the timing of its review of an application.
In addition, under the Pediatric Research Equity Act, or PREA, an NDA or supplement to an NDA must contain data that are adequate to assess the safety and effectiveness of the drug for the claimed indications in all relevant pediatric subpopulations, and to support dosing and administration for each pediatric subpopulation for which the product is safe and effective. The FDA may, on its own initiative or at the request of the applicant, grant deferrals for submission of some or all pediatric data until after approval of the product for use in adults, or full or partial waivers from the pediatric data requirements.
The FDA also may require submission of a risk evaluation and mitigation strategy, or REMS, to mitigate any identified or suspected serious risks and ensure safe use of the drug. The REMS plan could include medication guides, physician communication plans, assessment plans, and elements to assure safe use, such as restricted distribution methods, patient registries or other risk minimization tools.
The FDA conducts a preliminary review of all NDAs within the first 60 days after submission, before accepting them for filing, to determine whether they are sufficiently complete to permit substantive review. The FDA may request additional information rather than accept an NDA for filing. In this event, the application must be resubmitted with the additional information. The resubmitted application is also subject to review before the FDA accepts it for filing. Once the submission is accepted for filing, the FDA begins an in-depth substantive review. The FDA reviews an NDA to determine, among other things, whether the drug is safe and effective and whether the facility in which it is manufactured, processed, packaged or held meets standards designed to assure the product’s continued safety, quality and purity.
The FDA may refer an application for a novel drug to an external advisory committee. An advisory committee is a panel of independent experts, including clinicians and other scientific experts, that reviews, evaluates and provides a recommendation as to whether the application should be approved and under what conditions. The FDA is not bound by the recommendations of an advisory committee, but it considers such recommendations carefully when making decisions.
Before approving an NDA, the FDA typically will inspect the facility or facilities where the product is manufactured, referred to as a Pre-Approval Inspection. The FDA will not approve an application unless it determines that the manufacturing processes and facilities are in compliance with cGMP requirements and adequate to assure consistent production of the product within required specifications. Additionally, before approving an NDA, the FDA will typically inspect one or more clinical trial sites to assure compliance with cGCP.
The testing and approval process for an NDA requires substantial time, effort and financial resources, and each may take several years to complete. Data obtained from preclinical and clinical testing are not always conclusive and may be susceptible to varying interpretations, which could delay, limit or prevent regulatory approval. The FDA may not grant approval of an NDA on a timely basis, or at all.
26
After evaluating the NDA and all related information, including the advisory committee recommendation, if any, and inspection reports regarding the manufacturing facilities and clinical trial sites, the FDA may issue an approval letter, or, in some cases, a complete response letter. A complete response letter generally contains a statement of specific conditions that must be met in order to secure final approval of the NDA and may require additional clinical or preclinical testing in order for FDA to reconsider the application. Even with submission of this additional information, the FDA ultimately may decide that the application does not satisfy the regulatory criteria for approval. If and when those conditions have been met to the FDA’s satisfaction, the FDA may issue an approval letter. An approval letter authorizes commercial marketing of the drug with specific prescribing information for specific indications.
Even if the FDA approves a product, it may limit the approved indications for use of the product, require that contraindications, warnings or precautions be included in the product labeling, including a boxed warning, require that post-approval studies, including Phase 4 clinical trials, be conducted to further assess a drug’s safety after approval, require testing and surveillance programs to monitor the product after commercialization, or impose other conditions, including distribution restrictions or other risk management mechanisms under a REMS which can materially affect the potential market and profitability of the product. The FDA may prevent or limit further marketing of a product based on the results of post-marketing studies or surveillance programs. After approval, some types of changes to the approved product, such as adding new indications, manufacturing changes, and additional labeling claims, are subject to further testing requirements and FDA review and approval.
Breakthrough Therapy Designation. The FDA may expedite the review of a product candidate designated as a breakthrough therapy, which is intended, alone or in combination with one or more other drugs, to treat a serious or life-threatening disease or condition and preliminary clinical evidence indicates that the drug may demonstrate substantial improvement over existing therapies on one or more clinically significant endpoints, such as substantial treatment effects observed early in clinical development. A sponsor may request the FDA to designate a drug as a breakthrough therapy at the time of, or any time after, the submission of an IND application for the drug. If the FDA designates a drug as a breakthrough therapy, it must take actions appropriate to expedite the development and review of the application, which may include holding meetings with the sponsor and the review team throughout the development of the drug; providing timely advice to, and interactive communication with, the sponsor regarding the development of the drug to ensure that the development program to gather the nonclinical and clinical data necessary for approval is as efficient as practicable; involving senior managers and experienced review staff, as appropriate, in a collaborative, cross-disciplinary review; assigning a cross-disciplinary project lead for the FDA review team to facilitate an efficient review of the development program and to serve as a scientific liaison between the review team and the sponsor; and taking steps to ensure that the design of the clinical trials is as efficient as practicable, when scientifically appropriate, such as by minimizing the number of patients exposed to a potentially less efficacious treatment. The FDA may rescind a Breakthrough Therapy designation in the future if further clinical development later shows that the criteria for designation are no longer met. Breakthrough Therapy designation does not change the standards for approval, but may expedite the development or review process.
Post-Approval Requirements. Drugs manufactured or distributed pursuant to FDA approvals are subject to pervasive and continuing regulation by the FDA, including, among other things, requirements relating to recordkeeping, periodic reporting, product sampling and distribution, advertising and promotion, reporting of adverse experiences with the product, and compliance with any post-approval requirements imposed as a condition of approval, such as Phase 4 clinical trials and surveillance to assess safety and effectiveness after commercialization. After approval, most changes to the approved product, such as adding new indications or other labeling claims are subject to prior FDA review and approval. There also are continuing, annual program user fee requirements for any marketed products, as well as new application fees for supplemental applications with clinical data. In addition, drug manufacturers and other entities involved in the manufacture and distribution of approved drugs are required to register their establishments with the FDA and state agencies and are subject to periodic announced and unannounced inspections by the FDA and these state agencies for compliance with cGMP requirements. Changes to the manufacturing process are strictly regulated and often require prior FDA approval before being implemented. FDA regulations also require investigation and correction of any deviations from cGMP and impose reporting and documentation requirements upon the sponsor and any third-party manufacturers that the sponsor may decide to use. Accordingly, manufacturers must continue to expend time, money and effort in the area of production and quality control to maintain cGMP compliance.
27
Once an approval is granted, the FDA may withdraw the approval if compliance with regulatory requirements and standards is not maintained or if problems occur after the product reaches the market.
Later discovery of previously unknown problems with a product, including adverse events of unanticipated severity or frequency, or with manufacturing processes, or failure to comply with regulatory requirements, may result in mandatory revisions to the approved labeling to add new safety information; imposition of post-market studies or clinical trials to assess new safety risks; or imposition of distribution or other restrictions under a REMS program. Other potential consequences include, among other things:
| ● | restrictions on the marketing or manufacturing of the product, complete withdrawal of the product from the market or product recalls; |
| ● | fines, warning letters or holds on post-approval clinical trials; |
| ● | refusal of the FDA to approve pending NDAs or supplements to approved NDAs, or suspension or revocation of product license approvals; |
| ● | product seizure or detention, or refusal to permit the import or export of products; or |
| ● | injunctions or the imposition of civil or criminal penalties. |
The FDA strictly regulates marketing, labeling, advertising and promotion of products that are placed on the market. Although physicians, in the practice of medicine, may prescribe approved drugs for unapproved indications, pharmaceutical companies are required to promote their drug products only for the approved indications and in accordance with the provisions of the approved label. The FDA and other agencies actively enforce the laws and regulations prohibiting the promotion of off-label uses, and a company that is found to have improperly promoted off-label uses may be subject to significant liability. However, physicians may, in their independent medical judgment, prescribe legally available products for off-label uses. The FDA does not regulate the behavior of physicians in their choice of treatments but the FDA does restrict manufacturer’s communications on the subject of off-label use of their products.
In addition, the distribution of prescription pharmaceutical products is subject to the Prescription Drug Marketing Act, or PDMA, which regulates the distribution of drugs and drug samples at the federal level, and sets minimum standards for the registration and regulation of drug distributors by the states. Both the PDMA and state laws limit the distribution of prescription pharmaceutical product samples and impose requirements to ensure accountability in distribution.
Fraud and Abuse, Data Privacy and Security and Transparency Laws and Regulations
In addition to FDA restrictions on marketing of pharmaceutical products, federal and state health care regulatory laws restrict business practices in the biopharmaceutical industry. These laws include, among other things, anti-kickback and false claims laws and regulations, physician payment transparency laws and regulations, as well as data privacy and security laws and regulations.
The federal Anti-Kickback Statute prohibits, among other things, any person or entity, from knowingly and willfully offering, paying, soliciting or receiving any remuneration, directly or indirectly, overtly or covertly, in cash or in kind, to induce or in return for purchasing, leasing, ordering, or arranging for or recommending the purchase, lease, or order of any item or service reimbursable under Medicare, Medicaid or other federal healthcare programs. The term “remuneration” has been interpreted broadly to include anything of value. The Anti-Kickback Statute has been interpreted to apply to arrangements between pharmaceutical manufacturers on one hand and prescribers, purchasers, and formulary managers on the other. There are a number of statutory exceptions and regulatory safe harbors protecting some common activities from prosecution. Practices that involve remuneration that may be alleged to be intended to induce prescribing, purchases, or recommendations may be subject to scrutiny if they do not qualify for an exception or
28
safe harbor. Failure to meet all of the requirements of a particular applicable statutory exception or regulatory safe harbor does not make the conduct per se illegal under the Anti-Kickback Statute. Instead, the legality of the arrangement will be evaluated on a case-by-case basis based on a cumulative review of all of its facts and circumstances.
Additionally, the intent standard under the federal Anti-Kickback Statute was amended by the Patient Protection and Affordable Care Act, as amended by the Health Care Education Reconciliation Act (collectively, the “Health Care Reform Law”), to a stricter standard such that a person or entity no longer needs to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation. In addition, the Health Care Reform Law provided that the government may assert that a claim including items or services resulting from a violation of the federal Anti-Kickback Statute constitutes a false or fraudulent claim for purposes of the federal civil False Claims Act.
Federal false claims laws, including the federal civil False Claims Act prohibit, among other things, any person or entity from knowingly presenting, or causing to be presented, a false or fraudulent claim for payment to, or approval by, the federal government or knowingly making, using, or causing to be made or used a false record or statement material to a false or fraudulent claim to the federal government. A claim includes “any request or demand” for money or property presented to the U.S. government. The federal civil False Claims Act has been used to assert liability on the basis of kickbacks and other improper referrals, improperly reported government pricing metrics such as Best Price or Average Manufacturer Price, improper use of Medicare provider or supplier numbers when detailing a provider of services, improper promotion of off-label uses not expressly approved by FDA in a drug’s label, and allegations as to misrepresentations with respect to the services rendered. Additionally, the civil monetary penalties statute, which, among other things, imposes fines against any person or entity who is determined to have presented, or caused to be presented, claims to a federal healthcare program that the person knows, or should know, is for an item or service that was not provided as claimed or is false or fraudulent. The federal Health Insurance Portability and Accountability Act of 1996, or HIPAA, created additional federal criminal statutes that prohibit knowingly and willfully executing, or attempting to execute, a scheme to defraud or to obtain, by means of false or fraudulent pretenses, representations, or promises, any of the money or property owned by, or under the custody or control of, any healthcare benefit program, including private third-party payers and knowingly and willfully falsifying, concealing or covering up by trick, scheme or device a material fact or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services relating to healthcare matters. Also, many states have similar fraud and abuse statutes or regulations that apply to items and services reimbursed under Medicaid and other state programs, or, in several states, apply regardless of the payer.
In addition, we may be subject to data privacy and security regulation by both the federal government and the states in which we conduct our business. HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act, or HITECH, and their respective implementing regulations, including the Final HIPAA Omnibus Rule published on January 25, 2013, imposes specified requirements on certain types of individuals and entities subject to the law, known as covered entities, such as certain healthcare providers, health plans, and healthcare clearinghouses, as well as their business associates that process individually identifiable health information on their behalf, relating to the privacy, security and transmission of individually identifiable health information as well as their covered subcontractors. Among other things, HITECH makes security standards and certain privacy standards directly applicable to the business associates of covered entities that perform services for them that involve the creation, use, maintenance or disclosure of, individually identifiable health information. HITECH also created four new tiers of civil monetary penalties, amended HIPAA to make civil and criminal penalties directly applicable to business associates, and gave state attorneys general new authority to file civil actions for damages or injunctions in federal courts to enforce the federal HIPAA laws and seek attorney’s fees and costs associated with pursuing federal civil actions. In addition, state laws may govern the privacy and security of health information in certain circumstances, many of which differ from each other in significant ways and may not have the same effect, thus complicating compliance efforts.
Additionally, federal transparency laws, including the federal Physician Payments Sunshine Act created under Section 6002 of the Health Care Reform Law and its implementing regulations, require that manufacturers of drugs, devices, biologics and medical supplies for which payment is available under Medicare, Medicaid or the Children’s Health Insurance Program (with certain exceptions) report annually to the Centers for Medicare & Medicaid Services, or CMS, information related to payments or other transfers of value made or distributed to physicians (defined to include doctors of medicine, dentists, optometrists, podiatrists and chiropractors), other healthcare professionals (such as
29
physician assistants and nurse practitioners), and teaching hospitals, or to entities or individuals at their request or designation. Additionally, applicable manufacturers and applicable group purchasing organizations are required to report annually to CMS certain ownership and investment interests held by physicians (as defined above) and their immediate family members.
There are also an increasing number of analogous state laws that require manufacturers to file reports with states on pricing and marketing information, such as tracking and reporting of gifts, compensations, other remuneration and items of value provided to healthcare professionals and healthcare entities. For example, several states have enacted legislation requiring pharmaceutical companies to, among other things, establish and implement commercial compliance programs, file periodic reports with the state, make periodic public disclosures on sales, marketing, pricing, clinical trials and other activities and/or register their sales representatives. Certain state laws also regulate manufacturers’ use of prescriber-identifiable data. These laws may affect our sales, marketing and other promotional activities by imposing administrative and compliance burdens. In addition, given the lack of clarity with respect to these laws and their implementation, our reporting actions could be subject to the penalty provisions of the pertinent state and federal authorities.
If our operations are found to be in violation of any of the health regulatory laws described above or any other laws that apply to us, we may be subject to penalties, including significant criminal, civil and administrative penalties, damages, fines, imprisonment, exclusion from participation in government healthcare programs, contractual damages, reputational harm, diminished profits and future earnings, additional reporting requirements and/or oversight if we become subject to a corporate integrity agreement or similar agreement to resolve allegations of non-compliance with these laws, and the curtailment or restructuring of our operations, any of which could adversely affect our ability to operate our business and our results of operations. To the extent that any of our products are sold in a foreign country, we may be subject to similar foreign laws and regulations, which may include, for instance, applicable post-marketing requirements, including safety surveillance, anti-fraud and abuse laws, and implementation of corporate compliance programs and reporting of payments or transfers of value to healthcare professionals.
Coverage and Reimbursement Generally
The commercial success of KORSUVA injection and our ability to commercialize any approved product candidates successfully will depend in part on the extent to which governmental payer programs at the federal and state levels, including Medicare and Medicaid, private health insurers and other third-party payers provide coverage for and establish adequate reimbursement levels. In the United States, private health insurers and other third-party payers often provide reimbursement for products and services based on the level at which the government provides reimbursement through the Medicare or Medicaid programs for such products and services.
Patients who are prescribed treatments for their conditions and providers performing the prescribed services generally rely on third-party payers to reimburse all or part of the associated healthcare costs. In addition, many U.S. hospitals receive a fixed reimbursement amount per procedure for certain surgeries and other treatment therapies they perform, or a predetermined rate for all hospital inpatient care provided as payment in full. Because this amount may not be based on the actual expenses the hospital incurs, hospitals may choose to use therapies which are less expensive when compared to our product candidates. Sales of KORSUVA injection and our product candidates to the extent approved will therefore depend substantially, both domestically and abroad, on the extent to which the costs of our products will be paid by health maintenance, managed care, pharmacy benefit and similar healthcare management organizations, or reimbursed by government health administration authorities, such as Medicare and Medicaid, private health insurers and other third-party payers. Further, assuming coverage is approved, the resulting reimbursement payment rates might not be adequate. KORSUVA injection is expected to be designated as a component of the government’s bundled reimbursement for ESRD treatment.
Our U.S. commercial partner, Vifor Pharma Group, submitted the payment reimbursement application for TDAPA and HCPCS to CMS in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years.
30
Third-party payers are increasingly imposing additional requirements and restrictions on coverage and limiting reimbursement levels for medical products, including pharmaceuticals. For example, federal and state governments reimburse covered prescription drugs at varying rates generally below average wholesale price. These restrictions and limitations influence the purchase of healthcare services and products. Third-party payers may limit coverage to specific drug products on an approved list, or formulary, which might not include all of the FDA-approved drug products for a particular indication. Additionally, third-party payers are increasingly challenging the price and examining the medical necessity and cost-effectiveness of medical products and services, in addition to their safety and efficacy. Therefore, we may need to conduct expensive pharmacoeconomic studies in order to demonstrate the medical necessity and cost-effectiveness of our products, in addition to the costs required to obtain the FDA approvals. KORSUVA injection and any of our product candidates, to the extent they receive approval, may not be considered medically necessary or cost-effective. Moreover, a payer’s decision to provide coverage for a drug product does not imply that an adequate reimbursement rate will be approved, and one payer’s determination to provide coverage for a product does not assure that other payers will also provide coverage. Adequate third-party reimbursement may not be available to enable us to maintain price levels sufficient to realize an appropriate return on our investment in drug development. Legislative proposals to reform healthcare or reduce costs under government insurance programs may result in lower reimbursement for our products and product candidates or exclusion of our products and product candidates from coverage. The cost containment measures that healthcare payers and providers are instituting and any healthcare reform could significantly reduce our revenues from the sale of KORSUVA injection and any approved product candidates.
Healthcare Regulatory Developments
In the United States and some foreign jurisdictions, the legislative landscape with respect to healthcare continues to evolve. There have been a number of legislative and regulatory changes to the healthcare system that could affect our ability to sell our products profitably. Among policy makers and payers in the United States and elsewhere, there is significant interest in promoting changes in healthcare systems with the stated goals of containing healthcare costs, improving quality and expanding access. In the United States, the pharmaceutical industry has been a particular focus of these efforts and has been significantly affected by major legislative initiatives.
For example, the Health Care Reform Law was passed in March 2010 and includes provisions that have substantially changed healthcare financing by both governmental and private insurers. Among other provisions that could have an impact on our business, the Health Care Reform Law revised the methodology by which rebates owed by manufacturers to the state and federal government for covered outpatient drugs under the Medicaid Drug Rebate Program are calculated, increased the minimum Medicaid rebates owed by most manufacturers under the Medicaid Drug Rebate Program, extended the Medicaid Drug Rebate program to utilization of prescriptions of individuals enrolled in Medicaid managed care organizations, subjected manufacturers to new annual fees and taxes for certain branded prescription drugs, and provided incentives to programs that increase the federal government’s comparative effectiveness research. Additionally, the Health Care Reform Law implemented a new Medicare Part D coverage gap discount program in which manufacturers must now agree to offer 70% point-of-sale discounts off negotiated prices of applicable brand drugs to eligible beneficiaries during their coverage gap period as a condition for the outpatient drugs being covered under Medicare Part D.
There have been executive, judicial and Congressional challenges to certain aspects of the Health Care Reform Law. For example, the Tax Cuts and Jobs Act of 2017, or TCJA, included a provision that repealed, effective January 1, 2019, the tax-based shared responsibility payment imposed by the Health Care Reform Law on certain individuals who fail to maintain qualifying health coverage for all or part of a year that is commonly referred to as the “individual mandate”. On June 17, 2021, the U.S. Supreme Court dismissed a challenge on procedural grounds that argued the Health Care Reform Law is unconstitutional in its entirety because the “individual mandate” was repealed by Congress. Thus, the Health Care Reform Law will remain in effect in its current form. Prior to the U.S. Supreme Court ruling, on January 28, 2021, President Biden issued an executive order to initiate a special enrollment period from February 15, 2021 through August 15, 2021 for purposes of obtaining health insurance coverage through the Health Care Reform Law marketplace. The executive order also instructed certain governmental agencies to review and reconsider their existing policies and rules that limit access to healthcare, including among others, reexamining Medicaid demonstration projects and waiver programs that include work requirements, and policies that create unnecessary barriers to obtaining access to health insurance coverage through Medicaid or the Health Care Reform Law. It is possible that the Health Care Reform
31
Law will be subject to judicial or Congressional challenges in the future. It is unclear how such challenges and the healthcare reform measures of the Biden administration will impact the Health Care Reform Law and our business.
In addition, other legislative changes have been proposed and adopted since the Health Care Reform Law was enacted. In August 2011, President Obama signed into law the Budget Control Act of 2011, as amended, which, among other things, created the Joint Select Committee on Deficit Reduction to recommend proposals in spending reductions to Congress. The Joint Select Committee on Deficit Reduction did not achieve its targeted deficit reduction of at least $1.2 trillion for the years 2013 through 2021, triggering the legislation’s automatic reductions to several government programs. These reductions include aggregate reductions to Medicare payments to providers of up to 2% per fiscal year starting in 2013 and, due to subsequent legislative amendments, will remain in effect until 2031, except for a temporary suspension from May 1, 2020 through March 31, 2022 due to the COVID-19 pandemic, unless additional Congressional action is taken. Under current legislation, the actual reduction in Medicare payments will vary from 1% in 2022 to up to 3% in the final fiscal year of this sequester. In January 2013, President Obama signed into law the American Taxpayer Relief Act of 2012, which, among other things, further reduced Medicare payments to several providers and increased the statute of limitations period for the government to recover overpayments to providers from three to five years. Additionally, on March 11, 2021, President Biden signed the American Rescue Plan Act of 2021 into law, which eliminates the statutory Medicaid drug rebate cap, currently set at 100% of a drug’s average manufacturer price, for single source and innovator multiple source drugs, beginning January 1, 2024. Congress is considering additional health reform measures.
In the United States, the EU, and other potentially significant markets for our product candidates, government authorities and third-party payers are increasingly attempting to limit or regulate the price of medical products and services, particularly for new and innovative products and therapies, which often has resulted in average selling prices lower than they would otherwise be. Further, the increased emphasis on managed healthcare in the United States and on country and regional pricing and reimbursement controls in the EU will put additional pressure on product pricing, reimbursement and utilization, which may adversely affect our future product sales and results of operations. For example, there have been several recent U.S. Presidential executive orders, Congressional inquiries and proposed and enacted federal and state legislation designed to, among other things, bring more transparency to drug pricing, review the relationship between pricing and manufacturer patient programs, reduce the cost of drugs under Medicare, and reform government program reimbursement methodologies for drugs. At the federal level, the Trump administration used several means to propose or implement drug pricing reform, including through federal budget proposals, executive orders and policy initiatives. For example, on July 24, 2020 and September 13, 2020, the Trump administration announced several executive orders related to prescription drug pricing that seek to implement several of the administration’s proposals. As a result, the FDA concurrently released a final rule and guidance in September 2020, providing pathways for states to build and submit importation plans for drugs from Canada. Further, on November 20, 2020, HHS finalized a regulation removing safe harbor protection for price reductions from pharmaceutical manufacturers to plan sponsors under Part D, either directly or through pharmacy benefit managers, unless the price reduction is required by law. The implementation of the rule has been delayed by the Biden administration from January 1, 2022 to January 1, 2023 in response to ongoing litigation. The rule also creates a new safe harbor for price reductions reflected at the point-of-sale, as well as a safe harbor for certain fixed fee arrangements between pharmacy benefit managers and manufacturers, the implementation of which have also been delayed by the Biden administration until January 1, 2023. On November 20, 2020, CMS issued an interim final rule implementing President Trump’s Most Favored Nation executive order, which would tie Medicare Part B payments for certain physician-administered drugs to the lowest price paid in other economically advanced countries, effective January 1, 2021. As a result of litigation challenging the Most Favored Nation model, on December 27, 2021, CMS published a final rule that rescinds the Most Favored Nation model interim final rule. Additionally, in July 2021, the Biden administration released an executive order, “Promoting Competition in the American Economy,” with multiple provisions aimed at prescription drugs. In response to Biden’s executive order, on September 9, 2021, HHS released a Comprehensive Plan for Addressing High Drug Prices that outlines principles for drug pricing reform and sets out a variety of potential legislative policies that Congress could pursue as well as potential administrative actions HHS can take to advance these principles. No legislation or administrative actions have been finalized to implement these principles. It is unclear whether these or similar policy initiatives will be implemented in the future. At the state level, legislatures have increasingly passed legislation and implemented regulations designed to control pharmaceutical and biological product pricing, including price or patient reimbursement constraints, discounts, restrictions on certain product access and marketing cost
32
disclosure and transparency measures, and, in some cases, to encourage importation from other countries and bulk purchasing. These pressures can arise from rules and practices of managed care groups, judicial decisions and laws and regulations related to Medicare, Medicaid and healthcare reform, pharmaceutical coverage and reimbursement policies and pricing in general.
These and other healthcare reform initiatives may result in additional reductions in Medicare payments and other healthcare funding, which could have a material adverse effect on our financial operations. We expect that additional state and federal healthcare reform measures will be adopted in the future, any of which could limit the amounts that federal and state governments will pay for healthcare products and services, which could further limit the prices we are able to charge, or the amounts of reimbursement available, for KORSUVA injection and our product candidates once they are approved. Further, it is possible that additional governmental action is taken in response to the COVID-19 pandemic.
Foreign Regulation
In order to market any product outside of the United States, we would need to comply with numerous and varying regulatory requirements of other countries regarding safety and efficacy and governing, among other things, clinical trials, marketing authorization, commercial sales and distribution of our products. For example, in the EU, we must obtain authorization of a clinical trial application, or CTA, in each member state in which we intend to conduct a clinical trial. Whether or not we obtain FDA approval for a product, we would need to obtain the necessary approvals by the comparable regulatory authorities of foreign countries before we can commence clinical trials or marketing of the product in those countries. The approval process varies from country to country and can involve additional product testing and additional administrative review periods. The time required to obtain approval in other countries might differ from and be longer than that required to obtain FDA approval. Regulatory approval in one country does not ensure regulatory approval in another, but a failure or delay in obtaining regulatory approval in one country may negatively impact the regulatory process in others.
Employees and Human Capital
As of February 24, 2022, we had 84 employees, of whom 24 hold PharmD, PhD or MD degrees or the foreign equivalent. All of these employees are located in the United States. None of our employees are represented by a labor union or covered by a collective bargaining agreement. We consider our relationship with our employees to be good.
Our human capital resources objectives include, as applicable, identifying, recruiting, retaining, incentivizing, and integrating our existing and new employees, advisors, and consultants. The principal purposes of our equity and cash incentive plans are to attract, retain and reward personnel through the granting of stock-based and cash-based compensation awards, in order to increase stockholder value and the success of our company by motivating such individuals to perform to the best of their abilities and achieve our objectives.
Website Access to Reports
Our website is www.caratherapeutics.com. We are subject to the informational requirements of the Exchange Act and file or furnish reports, including our Annual Report on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K, and amendments to reports filed pursuant to Sections 13(a) and 15(d) of the Exchange Act, proxy statements and other information with the SEC. We make copies of these reports and other information available free of charge through our website (under the heading “SEC Filings”) as soon as reasonably practicable after we file or furnish them with the SEC. The SEC maintains a website that contains reports, proxy and information statements and other information regarding issuers that file electronically with the SEC at www.sec.gov. The information contained on the websites referenced in this Annual Report on Form 10-K is not incorporated by reference into this filing, and the website addresses are provided only as inactive textual references.
33
Item 1A. Risk Factors
In addition to other information contained in this Annual Report on Form 10-K, the following risks should be considered in evaluating our business and future prospects and an investment in our common stock. The risks and uncertainties described below are not the only ones we face. If any of the following risks and uncertainties develops into actual events, our business, financial condition, results of operations and cash flows could be materially adversely affected. In that case, the price of our common stock could decline and you may lose all or part of your investment.
Risks Related to Our Business and the Development and Commercialization of Our Product and Product Candidates
We are substantially dependent on the success of our product and product candidates. If we are unable to successfully complete clinical development, obtain additional regulatory approvals and commercialize our product and product candidates, or experience significant delays in doing so, our business will be materially harmed.
Our business depends on the successful development, regulatory approval and commercialization of our product, KORSUVA injection, and product candidates. In August 2021, the FDA approved KORSUVA injection for the treatment of moderate-to-severe CKD-aP in adults undergoing hemodialysis. Our partner, VFMCRP, submitted an MAA to the EMA in March 2021, which was accepted for review by the EMA. If approved, KORSUVA injection would receive marketing authorization in all member states of the EU, as well as in Iceland, Liechtenstein, and Norway. The EMA’s decision on the EU MAA is expected in the second quarter of 2022; however, we cannot assure you that the results of our trials will successfully support the additional regulatory applications for approval. Our ability to generate product revenues in the near term is dependent on our and our commercial partners’ ability to successfully commercialize KORSUVA injection. Although during the year ended December 31, 2021 we recognized commercial supply revenue of $0.7 million from the sale of KORSUVA injection to Vifor, we currently generate no revenues from sales of any products, and we may never be able to develop or successfully commercialize a marketable product.
KORSUVA injection in the U.S. will require marketing efforts by our commercial partners before we generate any revenues from product sales. For example, we submitted required documents to CMS to ensure timely reimbursement and patient access to KORSUVA injection. Vifor Pharma Group submitted the application for a HCPCS reimbursement code and the payment reimbursement application for a TDAPA to CMS in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years. CMS expressed in its written communication to us and Vifor Pharma, a continuing interest in engaging with the companies regarding potential post-TDAPA support to ensure all beneficiaries with ESRD have access to innovative products such as KORSUVA injection. However, there is no assurance that KORSUVA injection will be able to maintain its price established in the TDAPA period in the post-TDAPA timeframe. If we and our commercial partners do not successfully commercialize KORSUVA injection, we will not be able to generate revenue from sales of any products in the United States in the foreseeable future, or at all. Any significant delays in commercializing KORSUVA injection will have a substantial adverse impact on our business and financial condition.
Further, we cannot be certain that Oral KORSUVA (difelikefalin) or any future product candidates will be successful in clinical trials or receive regulatory approval. Regulatory authorities may interpret our data differently than we have. We are not permitted to market or promote any of our product candidates before we receive regulatory approval from the FDA or comparable foreign regulatory authorities, and we may never receive such regulatory approval for any of our product candidates.
The success of our products and product candidates depends on many factors, including but not limited to:
| ● | successful enrollment in, and completion of, clinical trials, as well as completion of preclinical studies; |
| ● | safety and favorable efficacy and acceptable safety data from our clinical trials and other studies; |
34
| ● | receipt of additional regulatory approvals; |
| ● | managing our reliance on sole-source third parties such as our third-party suppliers and manufacturers; |
| ● | the performance by CROs or other third parties we may retain of their duties to us in a manner that complies with our protocols and applicable laws and that protects the integrity of the resulting data; |
| ● | obtaining and maintaining patent, trade secret and other intellectual property protection and regulatory exclusivity; |
| ● | ensuring we do not infringe, misappropriate or otherwise violate the valid patent, trade secret or other intellectual property rights of third parties; |
| ● | successfully launching our product, such as KORSUVA injection, with our commercial partners, including market acceptance, and our other product candidates, if and when approved; |
| ● | obtaining and maintaining favorable reimbursement from third-party payers for products and product candidates; |
| ● | competition with other products; |
| ● | post-marketing commitments, if any, to regulatory agencies following regulatory approval of our product candidates; |
| ● | continued acceptable safety profile following regulatory approval; and |
| ● | manufacturing or obtaining sufficient supplies of our products and product candidates that may be necessary for use in clinical trials for evaluation of our product candidates and commercialization of our products. |
If we do not achieve and maintain one or more of these factors in a timely manner or at all, we could experience significant delays in our ability to, or be unable to obtain additional regulatory approvals for, and/or to successfully commercialize our products and product candidates, which would materially harm our business and we may not be able to generate sufficient revenues and cash flows to continue our operations.
We rely, and expect to continue to rely, on third parties to conduct our preclinical studies and clinical trials, and those third parties may not perform satisfactorily, including failing to meet deadlines for the completion of such trials.
We rely on third-party CROs to conduct our preclinical and clinical trials for all of our product candidates, and do not plan to independently conduct clinical trials of any other potential product candidates. We expect to continue to rely on third parties, such as CROs, clinical data management organizations, medical institutions and clinical investigators, to conduct our preclinical studies and clinical trials. These agreements might terminate for a variety of reasons, including a failure to perform by the third parties. If we need to enter into alternative arrangements, that would delay our product development activities and adversely affect our business.
Our reliance on these third parties for development activities will reduce our control over these activities. Nevertheless, we are responsible for ensuring that each of our studies is conducted in accordance with the applicable protocol, legal, regulatory and scientific standards and our reliance on the CROs does not relieve us of our regulatory responsibilities. For example, we will remain responsible for ensuring that each of our clinical trials is conducted in accordance with the general investigational plan and protocols for the trial and for ensuring that our preclinical trials are conducted in accordance with FDA’s good laboratory practice, or GLP, as appropriate. Moreover, the FDA and comparable foreign regulatory authorities require us to comply with standards, commonly referred to as good clinical practices, or GCPs, for conducting, recording and reporting the results of clinical trials to assure that data and reported results are credible and accurate and that the rights, integrity and confidentiality of trial participants are protected.
35
Regulatory authorities enforce these requirements through periodic inspections of trial sponsors, clinical investigators and trial sites. If we or any of our CROs fail to comply with applicable GCPs, the clinical data generated in our clinical trials may be deemed unreliable and the FDA or comparable foreign regulatory authorities may require us to perform additional clinical trials before approving our marketing applications. We cannot assure you that upon inspection by a given regulatory authority, such regulatory authority will determine that any of our clinical trials complies with GCP regulations. In addition, our clinical trials must be conducted with product produced, under current good manufacturing practices, or cGMP, regulations. Our failure to comply with these regulations may require us to repeat clinical trials, which would delay the regulatory approval process. We also are required to register certain clinical trials and post the results of certain completed clinical trials on a government-sponsored database, ClinicalTrials.gov, within specified timeframes. Failure to do so can result in fines, adverse publicity and civil and criminal sanctions.
Our CROs may also have relationships with other entities, some of which may be our competitors. In addition, our CROs are not our employees, and except for remedies available to us under our agreements with such CROs, we cannot control whether or not they devote sufficient time and resources to our on-going clinical, non-clinical and preclinical programs. In addition, the operations of our CROs may be constrained or disrupted by the ongoing COVID-19 pandemic. If these third parties do not successfully carry out their contractual duties, meet expected deadlines or conduct our preclinical studies or clinical trials in accordance with regulatory requirements or our stated protocols, if they need to be replaced or if the quality or accuracy of the clinical data they obtain is compromised due to the failure to adhere to our clinical protocols, regulatory requirements or for other reasons, our clinical trials may be extended, delayed or terminated and we may not be able to obtain, or may be delayed in obtaining, marketing approvals for our product candidates and will not be able to, or may be delayed in our efforts to, successfully commercialize our products and product candidates. As a result, our results of operations and the commercial prospects for our products and product candidates would be harmed, our costs could increase and our ability to generate revenues could be delayed.
If any of our relationships with these third-party CROs terminate, we may not be able to enter into arrangements with alternative CROs or to do so on commercially reasonable terms. Switching or adding additional CROs involves additional cost and requires management time and focus. In addition, there is a natural transition period when a new CRO commences work. As a result, delays could occur, which could compromise our ability to meet our desired development timelines. Though we carefully manage our relationships with our CROs, there can be no assurance that we will not encounter similar challenges or delays in the future or that these delays or challenges will not have a material adverse impact on our business, financial condition and prospects.
If the manufacturers upon whom we rely fail to produce our products or product candidates in the volumes that we require on a timely basis, or to comply with stringent regulations applicable to pharmaceutical drug manufacturers, we may face delays in the development and commercialization of, or be unable to meet demand for, our products and may lose potential revenues.
We do not manufacture KORSUVA injection or any of our product candidates, and we do not currently plan to develop any capacity to do so. We currently rely, and expect to continue to rely, on third parties for the manufacture of our products for commercialization and product candidates for preclinical and clinical testing. It is our intention that by the time of additional regulatory approvals for commercialization, we will have negotiated long-term commitments with at least one primary supplier for each manufacturing and distribution function. In July 2019, we entered into a non-exclusive commercial manufacturing agreement with Patheon for KORSUVA (difelikefalin) injection and in July 2021, we entered into a commercial supply agreement with Polypeptide Laboratories S.A., or PPL, for the KORSUVA (difelikefalin) injection. Any problems or delays we experience in preparing for commercial-scale manufacturing of a product or product candidate may result in a delay in FDA approval of the product candidate or may impair our ability to manufacture commercial quantities, which would adversely affect our business. For example, our manufacturers will need to produce specific batches of our products and product candidates to demonstrate acceptable stability under various conditions and for commercially viable lengths of time. We and our contract manufacturers will need to demonstrate to the FDA and other regulatory authorities this acceptable stability data for our products and product candidates, as well as validate methods and manufacturing processes, in order to receive and maintain regulatory approval to commercialize KORSUVA injection or any other product candidates. Furthermore, if our commercial manufacturers fail to deliver the required commercial quantities of bulk drug substance or finished product on a timely
36
basis and at commercially reasonable prices, we would likely be unable to meet demand for our products and we would lose potential revenues.
The manufacture of pharmaceutical products requires significant expertise and capital investment, including the development of advanced manufacturing techniques and process controls. Manufacturers of pharmaceutical products often encounter difficulties in production, particularly in scaling up initial production. These problems include difficulties with production costs and yields, quality control, including stability of the products and product candidate and quality assurance testing, shortages of qualified personnel, as well as compliance with strictly enforced federal, state and foreign regulations. Our manufacturers may not perform as agreed. If our manufacturers were to encounter any of these difficulties, our ability to provide products for commercialization and product candidates to patients in our clinical trials would be jeopardized. This could, among other things, lead to increased costs, lost revenue, damage to customer relationships, time and expense spent investigating the cause and, depending on the cause, similar losses with respect to other batches or products. If problems are not discovered before the product is released to the market, recall and product liability costs may also be incurred.
Further, we may rely on proprietary technology developed by our contract manufacturers for purposes of manufacturing certain of our products and product candidates and our failure to negotiate or maintain the long-term use of any such proprietary technology or the inability for our contract manufacturers to produce our products and product candidates or components of our products and product candidates in the volumes that we require on a timely basis, may lead to delays or interruptions in the regulatory approval or commercialization process, as well as increased costs. For example, in August 2019, we entered into the Enteris License Agreement and intend to use Enteris’s Peptelligence® technology to develop, manufacture and commercialize Oral KORSUVA (difelikefalin). If we experience any interruptions in the manufacture, delivery or scale-up of the Enteris formulation technology, we may experience delays in the development and commercialization of Oral KORSUVA (difelikefalin). Further, if we are unable to maintain our relationship with Enteris, we may be forced to reformulate Oral KORSUVA (difelikefalin) which could result in significantly delaying commercializing Oral KORSUVA (difelikefalin) and require us to incur additional costs in connection with such reformulation and potentially needed to seek additional approvals from the FDA. The operations of our third-party manufacturers have been and may in the future be constrained or disrupted and their operating capacity may be reduced by the ongoing COVID-19 pandemic, which could negatively impact our clinical development and commercialization timelines.
In addition, all manufacturers of our products and product candidates must comply with cGMP requirements enforced by the FDA through its facilities inspection program. These requirements include quality control, quality assurance and the maintenance of records and documentation. Manufacturers of our products and product candidates may be unable to comply with these cGMP requirements and with other FDA, state and foreign regulatory requirements. If our contract manufacturers cannot successfully manufacture material that conforms to our specifications and the strict regulatory requirements of the FDA or other regulatory authorities, they will not be able to secure and/or maintain regulatory approval for their manufacturing facilities. In addition, regulatory agencies subject an approved product, its manufacturer and the manufacturer’s facilities to continual review and inspections, including periodic unannounced inspections. The subsequent discovery of previously unknown problems with our current or any future approved products, including adverse events of unanticipated severity or frequency, or problems with the facilities where our current or any future approved products are manufactured, may result in restrictions on the marketing of our current or any such future approved products, up to and including withdrawal of the affected product from the market. We have little control over our manufacturers’ compliance with these regulations and standards. If the FDA or a comparable foreign regulatory authority does not approve these facilities for the manufacture of our products and product candidates or if it withdraws any such approval in the future, we may need to find alternative manufacturing facilities, which would significantly impact our ability to develop, obtain regulatory approval for or market our products and product candidates, if approved. A failure to comply with these requirements may result in fines and civil penalties, suspension of production, suspension, delay or denial of product approval, product seizure or recall, or withdrawal of product approval. If the safety of any quantities supplied is compromised due to our manufacturers’ failure to adhere to applicable laws or for other reasons, we may not be able to obtain regulatory approval for or successfully commercialize our products and product candidates.
37
Even if we obtain additional regulatory approvals for our product candidates, they may never be successfully launched or become profitable, in which case our business, prospects, operating results and financial condition may be materially harmed.
In order to successfully launch our products and product candidates and have them become profitable, we anticipate that we will have to dedicate substantial time and resources. Our ability to generate revenues from our commercialized products will depend on a number of factors, including, but not limited to:
| ● | achievement of broad market acceptance and coverage by third-party payers for our products; |
| ● | our partners’ effectiveness in marketing and selling our products; |
| ● | our ability to have manufactured commercial quantities of our products at acceptable cost levels and in compliance with regulatory requirements; |
| ● | our ability to maintain a cost-efficient organization and, to the extent we seek to do so, to collaborate successfully with additional third parties; |
| ● | our ability to expand and maintain intellectual property protection for our products successfully; |
| ● | the efficacy and safety of our products; and/or |
| ● | our ability to comply with regulatory requirements, which are subject to change. |
Because of the numerous risks and uncertainties associated with our commercialization efforts, we may not be able to achieve profitability. Even if we do achieve profitability, we may not be able to sustain or increase profitability on a quarterly or annual basis. A failure to become and remain profitable would depress the value of our company and could impair our ability to raise capital, expand our business, diversify our product offerings or continue our operations. A decline in the value of our company could also cause you to lose all or part of your investment.
If we or our collaborators are unable to establish effective marketing and sales capabilities, or if we are unable to enter into or maintain agreements with third parties to market and sell our products and product candidates, if they are approved, we may be unable to generate product revenues.
We currently do not have an internal commercial infrastructure for the marketing, sale and distribution of pharmaceutical products. In order to commercialize our product and product candidates (if approved), we must build our marketing, sales and distribution capabilities or make and maintain arrangements with third parties to perform these services. We have no prior experience in the marketing, sale and distribution of pharmaceutical products, and there are significant risks involved in the building and managing of a commercial infrastructure to the extent we choose to do so in the future. The establishment and development of our own sales force and related plans to market any products we may develop will be expensive and time consuming and could delay any product launch, and we may not be able to successfully develop this capability.
In August 2021, the FDA approved KORSUVA injection for the treatment of moderate-to-severe CKD-AP in adults undergoing hemodialysis in the U.S. We have entered into agreements with Vifor and VFMCRP to commercialize KORSUVA injection in the U.S. We are dependent on Vifor and VFMCRP to successfully commercialize KORSUVA injection with their own, or their collaborators’, sales force. We have partnered with VFMCRP to commercialize KORSUVA worldwide (if and when approved), excluding Japan (Maruishi/sub-licensee Kissei), and South Korea (CKDP). We and Vifor began commercializing KORSUVA injection in the U.S. in December 2021 and we expect commercial launch of KORSUVA injection in April 2022 and associated revenues in the second quarter of 2022.
We, or our partners or collaborators, will have to compete with other pharmaceutical and biotechnology companies to recruit, hire, train, manage and retain marketing and sales personnel. In the event that we or our partners or our
38
collaborators are unable to develop a marketing and sales infrastructure, we may not be able to commercialize KORSUVA injection or any of our other current or future product candidates, which would limit our ability to generate product revenues. Factors that may inhibit our or our partners’ or collaborators’ efforts to commercialize KORSUVA injection or our other current or future product candidates include:
| ● | inability to recruit, train, manage and retain adequate numbers of effective sales and marketing personnel; |
| ● | inability of sales personnel to obtain access to physicians or educate adequate numbers of physicians on the benefits of prescribing KORSUVA injection or our other current or future product candidates; |
| ● | inability to effectively oversee a geographically dispersed sales and marketing team; |
| ● | the lack of complementary products to be offered by sales personnel, which may put us at a competitive disadvantage relative to companies with more extensive product lines; and |
| ● | unforeseen costs and expenses associated with creating an independent sales and marketing organization. |
Our or our partners’ or our collaborators’ sales force and marketing teams may not be successful in commercializing KORSUVA injection or any of our other current or future product candidates.
In the event that we are unable to successfully collaborate with a third-party marketing and sales organization to commercialize any approved product candidates outside the United States, our ability to generate product revenues may be limited. To the extent that we rely on third parties to commercialize products for which we obtain regulatory approval, we may receive less revenues than if we commercialized these products ourselves. In addition, we would have less control over the sales efforts of any other third parties involved in our commercialization efforts.
We face significant competition from other pharmaceutical and biotechnology companies, academic institutions, government agencies and other research organizations. Our operating results will suffer if we fail to compete effectively.
The development and commercialization of new drug products is highly competitive. We face competition with respect to our current products and product candidates and will face competition with respect to any product candidates that we may seek to develop or commercialize in the future, from major pharmaceutical companies, specialty pharmaceutical companies and biotechnology companies worldwide. There are a number of large pharmaceutical and biotechnology companies that currently market and sell products or are pursuing the development of products for the treatment of pain and pruritus. Potential competitors also include academic institutions, government agencies and other public and private research organizations that conduct research, seek patent protection and establish collaborative arrangements for research, development, manufacturing and commercialization.
Among the companies that currently market or are developing therapies in the pruritus space that, if approved, our products and product candidates may potentially compete with include: Pfizer, AbbVie, Eli Lilly, Amgen, Regeneron, Leo Pharma, Galderma, Chugai, Trevi and others.
Our commercial opportunity could be reduced or eliminated if our competitors develop and commercialize products that are safer, more effective, have fewer or less severe side effects, are more convenient or are less expensive than our products or our current or future product candidates. Our competitors also may obtain FDA or other regulatory approval for their products more rapidly than we may obtain approval for ours, which could result in our competitors establishing a strong market position before we are able to enter the market. In addition, our ability to compete may be affected in many cases by insurers or other third-party payers seeking to encourage the use of generic products. Generic products are currently on the market for some of the indications that we are pursuing, and additional products are expected to become available on a generic basis over the coming years. We expect that KORSUVA injection, and our product candidates (if approved), will be priced at a significant premium over competitive generic products.
39
Many of the companies against which we are competing or against which we may compete in the future have significantly greater financial resources and expertise in R&D, manufacturing, preclinical testing, conducting clinical trials, obtaining regulatory approvals and marketing approved products than we do. Mergers and acquisitions in the pharmaceutical and biotechnology industries may result in even more resources being concentrated among a smaller number of our competitors. Early-stage companies may also prove to be significant competitors, particularly through collaborative arrangements with large and established companies. These third parties compete with us in recruiting and retaining qualified scientific and management personnel, establishing clinical trial sites and patient registration for clinical trials, as well as in acquiring technologies complementary to, or necessary for, our programs.
To the extent that KORSUVA injection or our product candidates, if approved, do not achieve broad market acceptance, the revenues that we generate from sales will be limited.
We have never successfully commercialized a product or product candidate for any indication. KORSUVA injection and our other current or future product candidates, if approved by the appropriate regulatory authorities for marketing and sale, may not gain acceptance among physicians, hospitals, dialysis providers, patients and third-party payers. If KORSUVA injection and any product candidates for which we obtain regulatory approval do not gain an adequate level of market acceptance, we may not generate significant product revenues or become profitable. Market acceptance of KORSUVA injection, Oral KORSUVA (difelikefalin) and any future product candidate by physicians, hospitals, dialysis providers, patients and third-party payers will depend on a number of factors, some of which are beyond our control. The degree of market acceptance of KORSUVA injection and any of our product candidates will depend on a number of factors, including:
| ● | the prevalence and severity of adverse events associated with such product or product candidate; |
| ● | limitations or warnings contained in the product’s FDA-approved labeling, including potential limitations or warnings for such product candidate, that may be more restrictive than other pain management or pruritus products; |
| ● | changes in the standard of care for the targeted indications for such product candidate, which could reduce the marketing impact of any claims that we could make following additional FDA approval, if obtained; |
| ● | the relative convenience and ease of administration of such product or product candidate; |
| ● | cost of treatment versus economic and clinical benefit in relation to alternative treatments or therapies; |
| ● | the availability of coverage and adequate reimbursement by third-party payers, such as insurance companies and other healthcare payers, and by government healthcare programs, including Medicare and Medicaid; |
| ● | the extent and strength of our marketing and distribution of such product or product candidate; |
| ● | the safety, efficacy and other potential advantages over, and availability of, alternative treatments already used to treat acute pain, chronic pain and/or pruritus; |
| ● | distribution and use restrictions, if any, imposed by the FDA with respect to such product candidate or to which we agree as part of a mandatory risk evaluation and mitigation strategy or voluntary risk management plan; |
| ● | the timing of market introduction of such product or product candidate, as well as competitive products; |
| ● | our ability to offer such product or product candidate for sale at competitive prices; |
| ● | the willingness of the target patient population to try new therapies and of physicians to prescribe these therapies; and |
40
| ● | the clinical indications for such product or product candidate if approved. |
Our and our commercial partners’ ability to effectively promote and sell KORSUVA injection and our current and future product candidates, if approved, will also depend on pricing and cost effectiveness, including our ability to produce a product at a competitive price and achieve acceptance of the product onto dialysis organization or hospital formularies, and our ability to obtain sufficient third-party coverage or reimbursement. Generally, before we or our commercial partners can attempt to sell a product in a hospital or dialysis provider, it must be approved for addition to that institution’s list of drugs approved for use in that institution, or formulary list. In evaluating drugs for inclusion on the formulary list, hospitals and dialysis providers evaluate a variety of factors, including cost. The frequency with which hospitals and dialysis providers add and remove drugs from their formulary lists varies from organization to organization, and institutions often require additional information prior to adding new drugs to their formulary, which may result in substantial delays in our receiving formulary approval for KORSUVA injection. Since most hospitals are members of group purchasing organizations, which leverage the purchasing power of a group of entities to obtain discounts based on the collective buying power of the group, our and our commercial partners’ ability to access customers in the hospital marketplace will also depend on our ability to effectively promote KORSUVA injection and our product candidates to group purchasing organizations. We will also need to demonstrate acceptable evidence of safety and efficacy, as well as relative convenience and ease of administration. Market acceptance could be limited depending on the prevalence and severity of any expected or unexpected adverse side effects associated with KORSUVA injection and our product candidates.
In addition, the potential market opportunity for KORSUVA injection and for our product candidates is difficult to precisely estimate. Our internal estimates of the potential market opportunity for our products and product candidates include several key assumptions based on our industry knowledge, industry publications, third-party research reports, assessment of competition, and other surveys. While we believe that our internal assumptions are reasonable, no independent source has verified such assumptions. If any of these assumptions proves to be inaccurate, then the actual market for our products and product candidates could be smaller than our estimates of our potential market opportunity. If the actual market for our products and product candidates is small, and/or smaller than we expect, our product revenue may be limited and it may be more difficult for us to achieve or maintain profitability.
Our and our commercial partners’ efforts to educate the medical community and third-party payers on the benefits of KORSUVA injection and our product candidates may require significant resources and may never be successful. Even if the medical community accepts that KORSUVA injection or one of our product candidates is safe and effective for its approved indications, physicians and patients may not immediately be receptive to such product or product candidate and may be slow to adopt it as an accepted treatment of pain or pruritus. It is unlikely that any future labeling approved by the FDA will contain claims that one of our products or product candidates is safer or more effective than competitive products or will permit us to promote such products or product candidate as being superior to competing products. Further, the availability of inexpensive generic forms of products for acute and chronic pain as well as pruritus may also limit acceptance of KORSUVA injection and our product candidates among physicians, patients and third-party payers. If KORSUVA injection and our current and any future product candidate, if approved, does not achieve an adequate level of acceptance among physicians, patients and third-party payers, we may not generate meaningful revenues from KORSUVA injection or our current and future product candidates, and we may not become profitable.
We face potential product liability exposure, and if successful claims are brought against us, we may incur substantial liability for KORSUVA injection or our other current and future product candidates that we may develop and may have to limit their commercialization.
We face an inherent risk of product liability lawsuits related to the sale of our products to, use of our products by, and testing of our product candidates in, seriously ill patients. For example, product liability claims might be brought against us by consumers, healthcare providers or others using, administering or selling our products. We may be sued if any product we develop allegedly causes injury or is found to be otherwise unsuitable during clinical testing, manufacturing, marketing or sale. Any such product liability claims may include allegations of defects in manufacturing, defects in design, a failure to warn of dangers inherent in the product, negligence, strict liability or a breach of
41
warranties. If we cannot successfully defend ourselves against these claims, we will incur substantial liabilities. Regardless of merit or eventual outcome, liability claims may result in:
| ● | loss of revenue from decreased demand for our products and/or product candidates; |
| ● | impairment of our business reputation or financial stability; |
| ● | costs of related litigation; |
| ● | substantial monetary awards to patients or other claimants; |
| ● | diversion of management attention and scientific resources from our business operations; |
| ● | withdrawal of clinical trial participants and potential termination of clinical trial sites or entire clinical programs; |
| ● | the inability to successfully commercialize our products and/or product candidates; |
| ● | significant negative media attention; |
| ● | initiation of investigations by regulators or increased regulatory scrutiny; |
| ● | product recalls, withdrawals or labeling, marketing or promotional restrictions; and |
| ● | the inability to commercialize our product candidates. |
With respect to KORSUVA injection and any of our other product candidates that are approved for commercial sale, we are, and will be, highly dependent upon physician and patient perceptions of us and the safety and quality of our products. We could be adversely affected if we are subject to negative publicity. We could also be adversely affected if any of our products or any similar products distributed by other companies prove to be, or are asserted to be, harmful to patients. Because of our dependence upon consumer perceptions, any adverse publicity associated with illness or other adverse effects resulting from patients’ use or misuse of our products or any similar products distributed by other companies could have a material adverse impact on our financial condition or results of operations.
We have obtained limited product liability insurance coverage for our products and our clinical trials with a $10.0 million annual aggregate coverage limit in the United States and various other coverage limits outside of the United States. However, our insurance coverage may not reimburse us or may not be sufficient to reimburse us for any expenses or losses we may suffer. Moreover, insurance coverage is becoming increasingly expensive, and, in the future, we may not be able to maintain insurance coverage at a reasonable cost or in sufficient amounts to protect us against losses due to liability. We intend to expand our insurance coverage to include the sale of commercial products for our product candidates in development, but we may be unable to obtain commercially reasonable product liability insurance for any products approved for marketing, or at all. On occasion, large judgments have been awarded in class action lawsuits based on drugs that had unanticipated side effects. A successful product liability claim or series of claims brought against us could cause our stock price to fall and, if judgments exceed our insurance coverage, could decrease our cash and adversely affect our business.
Our business, operations and clinical development and regulatory timelines and plans have been, and could continue to be, adversely affected by the effects of health epidemics, including the ongoing COVID-19 pandemic.
Our business, operations and clinical development timelines and plans have been, and could continue to be, adversely affected by health epidemics in regions where we have concentrations of third-party manufacturers, clinical trial sites or other business operations, and could cause significant disruption in the operations of third-party manufacturers or CROs upon whom we rely. In response to the ongoing COVID-19 pandemic, many state, local and
42
foreign governments have put in place, and continue to enforce in full or in part, quarantines, executive orders, shelter-in-place orders and similar government orders and restrictions in order to control the spread of the disease and its variants. Such orders or restrictions, and the perception that such orders or restrictions could occur, have resulted in business closures, work stoppages, slowdowns and delays, work-from-home policies, travel restrictions and cancellation of events, among other effects that have negatively impacted the global economy and could disrupt our business and operations. We have implemented a work-from-home policy for all employees, and we may take further actions that alter our operations as may be required by federal, state or local authorities, or which we determine are in the best interests of our employees. Moreover, our clinical development and regulatory timelines and plans could be affected by the ongoing COVID-19 pandemic. Site initiation and patient enrollment has been, and could in the future be, affected and some patients may not be able to comply with clinical trial protocols and the ability to conduct follow up visits with treated patients may be limited if quarantines impede patient movement or interrupt healthcare services. For example, the COVID-19 pandemic has affected the initiation of certain trial sites and patient enrollment for certain of our clinical trials, including our ongoing Phase 2 clinical trials of Oral KORSUVA (difelikefalin) for NP and for the treatment of pruritus in patients with hepatic impairment due to PBC. Similarly, our ability to recruit and retain patients and principal investigators and site staff who, as healthcare providers, may have heightened exposure to COVID-19 could be adversely impacted. Furthermore, our third-party manufacturers may be shut down or have difficulty meeting their contractual obligations, which may disrupt commercial and clinical drug supply chain continuity and the commercial launch of KORSUVA injection. In addition, COVID-19 may cause our third-party manufacturers of KORSUVA injection to operate at reduced capacity. While we currently do not expect any significant delays in our clinical development or commercial timelines, the ultimate impact of the evolving COVID-19 pandemic remains difficult to predict.
Further, the spread of COVID-19, which has caused a broad impact globally, may materially affect us economically. While the potential economic impact brought by and the duration of COVID-19 may be difficult to assess or predict, a widespread pandemic could result in significant disruption of global financial markets, reducing our ability to access capital, which could in the future negatively affect our liquidity. In addition, a recession or market correction resulting from the spread of COVID-19 could materially affect our business and the value of our common stock.
The global COVID-19 pandemic continues to rapidly evolve, and we will continue to monitor the COVID-19 situation closely. The ultimate impact of the COVID-19 pandemic or a similar health epidemic is highly uncertain and subject to change. We do not yet know the full extent of the potential impacts on our business, our clinical trials, healthcare systems or the global economy as a whole.
We may expend our limited resources to pursue a particular product candidate or indication and fail to capitalize on product candidates or indications that may be more profitable or for which there is a greater likelihood of success.
Because we have limited financial and managerial resources, we focus on developing product candidates for specific indications that we identify as most likely to succeed, in terms of both its regulatory approval and commercialization. As such, we are currently primarily focused on the development of Oral KORSUVA (difelikefalin) for AD-aP, NDD-CKD, CLD-PBC and NP. Further, at this time, we have de-prioritized the PONV program, as part of our strategy to focus on pruritus. As a result, we may have foregone or delayed, or may in the future forgo or delay, pursuit of opportunities with other product candidates or for other indications that may prove to have greater commercial potential. Our resource allocation decisions may cause us to fail to capitalize on viable commercial products or profitable market opportunities. Our spending on current and future R&D programs and product candidates for specific indications may not yield any commercially viable products. If we do not accurately evaluate the commercial potential or target market for a particular product candidate, we may relinquish valuable rights to that product candidate through collaboration, licensing or other royalty arrangements in cases in which it would have been more advantageous for us to retain sole development and commercialization rights to such product candidate.
43
Our future growth may depend on our ability to identify and develop products and if we do not successfully identify and develop product candidates or integrate them into our operations, we may have limited growth opportunities.
A component of our business strategy is to continue to develop a pipeline of product candidates by developing products that we believe are a strategic fit with our focus on pain and pruritus therapeutics. However, these business activities may entail numerous operational and financial risks, including:
| ● | difficulty or inability to secure financing to fund development activities for such development; |
| ● | disruption of our business and diversion of our management’s time and attention; |
| ● | higher than expected development costs; |
| ● | exposure to unknown liabilities; |
| ● | difficulty in managing multiple product development programs; and |
| ● | inability to successfully develop new products or clinical failure. |
We have limited resources to identify and execute the development of products. Moreover, we may devote resources to potential development that are never completed, or we may fail to realize the anticipated benefits of such efforts. If we do not successfully develop and commercialize product candidates, we may not be able to obtain product revenues in future periods.
The regulatory approval processes of the FDA and comparable foreign authorities are lengthy, time consuming and inherently unpredictable. If we are not able to obtain, or if there are delays in obtaining, required additional regulatory approvals, we will not be able to commercialize our product candidates as expected, and our ability to generate revenue will be materially impaired.
The time required to obtain approval by the FDA and comparable foreign authorities is unpredictable but typically takes many years following the commencement of clinical trials and depends upon numerous factors, including the substantial discretion of the regulatory authorities. In addition, approval policies, regulations, or the type and amount of clinical data necessary to gain approval may change during the course of a product candidate’s clinical development and may vary among jurisdictions. In August 2021, the FDA approved KORSUVA injection for the treatment of moderate-to-severe CKD-aP in adults undergoing hemodialysis in the U.S. Our partner, VFMCRP, submitted an MAA to the EMA in March 2021. We have not obtained regulatory approval for our other product candidates and it is possible that none of our existing product candidates, including KORSUVA injection in the EMA and Oral KORSUVA (difelikefalin), or any product candidates we may seek to develop in the future, will ever obtain regulatory approval.
Our product candidates and the activities associated with their development and commercialization, including their design, testing, manufacture, safety, efficacy, recordkeeping, labeling, storage, approval, advertising, promotion, sale and distribution, are subject to comprehensive regulation by the FDA and other regulatory agencies in the United States and by the EMA, and similar regulatory authorities outside the United States. Failure to obtain marketing approval for a product candidate will prevent us from commercializing that product candidate. We expect to continue to rely on third-party CROs and consultants to assist us in filing and supporting the applications necessary to gain marketing approvals. Securing marketing approval requires the submission of extensive preclinical and clinical data and supporting information to regulatory authorities for each therapeutic indication to establish the product candidate’s safety and efficacy for that indication. Securing marketing approval also requires the submission of information about the product manufacturing process to, and inspection of manufacturing facilities by, the regulatory authorities.
Clinical testing is expensive and can take many years to complete, and its outcome is inherently uncertain. Failure can occur at any time during the clinical trial process. The results of preclinical studies and early clinical trials of our product candidates may not be predictive of the results of later-stage clinical trials. Product candidates in later stages of
44
clinical trials may fail to show the desired safety and efficacy traits despite having progressed through preclinical studies and initial clinical trials. A number of companies in the biopharmaceutical industry have suffered significant setbacks in advanced clinical trials due to lack of efficacy or adverse safety profiles, notwithstanding promising results in earlier trials. Our future clinical trial results may not be successful. We may also experience numerous unforeseen events during, or as a result of, clinical trials that could delay or prevent our ability to receive marketing approval or commercialize our product candidates, including:
| ● | regulators or institutional review boards may not authorize us or our investigators to commence a clinical trial or conduct a clinical trial at a prospective trial site; |
| ● | we may experience delays in reaching, or fail to reach, agreement on acceptable clinical trial contracts or clinical trial protocols with prospective trial sites; |
| ● | clinical trials of our product candidates may produce negative or inconclusive results, and we may decide, or regulators may require us, to conduct additional clinical trials or abandon product development programs; |
| ● | the number of patients required for clinical trials of our product candidates may be larger than we anticipate, enrollment in these clinical trials may be slower than we anticipate or participants may drop out of these clinical trials at a higher rate than we anticipate; |
| ● | our third-party contractors may fail to comply with regulatory requirements or meet their contractual obligations to us in a timely manner, or at all; |
| ● | we may have to suspend clinical trials, as in the case of the IND clinical hold placed on our adaptive Phase 3 trial of I.V. difelikefalin for postoperative pain in February 2016, which was subsequently removed in April 2016, or terminate clinical trials of our product candidates for various reasons, including a finding that the participants are being exposed to unacceptable health risks; |
| ● | regulators or institutional review boards may require that we or our investigators suspend or terminate clinical research for various reasons, including noncompliance with regulatory requirements or a finding that the participants are being exposed to unacceptable health risks; |
| ● | changes in marketing approval policies during the development period; |
| ● | changes in or the enactment of additional statutes or regulations; |
| ● | changes in regulatory review for each submitted product application; |
| ● | the cost of clinical trials of our product candidates may be greater than we anticipate; |
| ● | the supply or quality of our product candidates or other materials necessary to conduct clinical trials of our product candidates may be insufficient or inadequate; and |
| ● | our product candidates may have undesirable side effects or other unexpected characteristics, causing us or our investigators, regulators or institutional review boards to suspend or terminate the trials. |
In addition, unfavorable changes in our industry or the global economy, including as a result of the ongoing COVID-19 pandemic, could contribute to some of the events listed above and further impact our ability to progress our clinical trials, submit for marketing approval or commercialize our product candidates, if approved, as planned. Further, if and to the extent, global health concerns prevent the FDA or other regulatory authorities from conducting their regular inspections, reviews, or other regulatory activities, it could significantly impact the ability of the FDA or other regulatory authorities to timely review and process our additional regulatory submissions, which could affect our ability
45
to obtain marketing approval for any of our product candidates, including our MAA to the EMA submitted in March 2021.
Moreover, if we are required to conduct additional clinical trials or other testing of our product candidates beyond those that we currently contemplate, if we are unable to successfully complete clinical trials of our product candidates or other testing, if the results of these trials or tests are not positive or are only modestly positive or if there are safety concerns, we may:
| ● | be delayed in obtaining marketing approval for our product candidates; |
| ● | not obtain marketing approval at all; |
| ● | obtain approval for indications or patient populations that are not as broad as intended or desired; |
| ● | obtain approval with labeling that includes significant use or distribution restrictions or safety warnings; |
| ● | be subject to additional post-marketing testing requirements; or |
| ● | have the product removed from the market after obtaining marketing approval. |
Furthermore, regulatory authorities have substantial discretion in the approval process and may refuse to accept any application or may decide that our data is insufficient for approval and require additional preclinical, clinical or other studies, including with respect to third-party technology used in any of our product candidates such as the excipient we intend to use for Oral KORSUVA (difelikefalin). In addition, varying interpretations of the data obtained from preclinical and clinical testing could delay, limit or prevent marketing approval of a product candidate. Any marketing approval we ultimately obtain may be limited or subject to restrictions or post-approval commitments that render the approved product not commercially viable.
Finally, even if we were to obtain approval, regulatory authorities may approve any of our product candidates for fewer or more limited indications than we request, may grant approval contingent on the performance of costly post-marketing clinical trials, or may approve a product candidate with a label that does not include the labeling claims necessary or desirable for the successful commercialization of that product candidate. Any of these scenarios could compromise the commercial prospects for our product candidates to assure safe use of the product candidates, either as a condition of product candidate approval or on the basis of new safety information.
If we experience delays in obtaining approval, if we fail to obtain approval of a product candidate or if the label for a product candidate does not include the labeling claims necessary or desirable for the successful commercialization of that product candidate, the commercial prospects for such product candidate may be harmed and our ability to generate revenues will be materially impaired.
For our approved product, KORSUVA injection, we will be subject to ongoing obligations and continued regulatory review, which may result in significant additional expense. Additionally, our product candidates, if approved, could be subject to labeling and other restrictions and market withdrawal and we may be subject to penalties if we fail to comply with regulatory requirements or experience unanticipated problems with our products.
KORSUVA injection and any product candidate for which we obtain marketing approval, along with the manufacturing processes, post-approval clinical data (if any), labeling, packaging, distribution, adverse event reporting, storage, recordkeeping, export, import, advertising and promotional activities for such product, will be subject to extensive and ongoing requirements of and review by the FDA and other regulatory authorities. These requirements include submissions of safety and other post-marketing information and reports, registration and listing requirements, continued compliance with cGMP requirements relating to manufacturing, quality control, quality assurance and corresponding maintenance of records and documents, requirements regarding the distribution of samples to physicians and recordkeeping and cGCPs for any clinical trials that we conduct post-approval. Even if marketing approval of a
46
product candidate is granted, the approval may be subject to limitations on the indicated uses for which the product may be marketed or to the conditions of approval, including any requirement to implement a Risk Evaluation and Mitigation Strategies, or REMS. If any of our product candidates receives marketing approval, the accompanying label may limit the approved use of our drug, which could limit sales of the product.
The FDA may also impose requirements for costly post-marketing studies or clinical trials and surveillance to monitor the safety or efficacy of the product. The FDA closely regulates the post-approval marketing and promotion of drugs to ensure drugs are marketed only for the approved indications and in accordance with the provisions of the approved labeling. The FDA imposes stringent restrictions on manufacturers’ communications regarding off-label use and if we do not market our products for their approved indications, we may be subject to enforcement action for off-label marketing. Violations of the Federal Food, Drug, and Cosmetic Act relating to the promotion of prescription drugs may lead to investigations alleging violations of federal and state health care fraud and abuse laws, as well as state consumer protection laws.
In addition, later discovery of previously unknown adverse events or other problems with our products, manufacturers or manufacturing processes, or failure to comply with regulatory requirements, may yield various results, including:
| ● | restrictions on the products, manufacturers, manufacturing facilities or manufacturing process; |
| ● | imposition of restrictions on operations, including costly new manufacturing requirements; |
| ● | restrictions on the labeling or marketing of a product; |
| ● | restrictions on product distribution or use; |
| ● | requirements to conduct post-marketing studies or clinical trials; |
| ● | warning letters; |
| ● | withdrawal of the products from the market; |
| ● | refusal to approve pending applications or supplements to approved applications that we submit; |
| ● | recall of products and publicity requirements; |
| ● | fines, restitution or disgorgement of profits or revenues; |
| ● | suspension or withdrawal of marketing or regulatory approvals; |
| ● | refusal to permit the import or export of our products; |
| ● | product seizure, detentions or import bans; or |
| ● | injunctions or the imposition of civil or criminal penalties. |
The FDA’s policies may change and additional government regulations may be enacted that could prevent, limit or delay regulatory approval of our product candidates. If we are slow or unable to adapt to changes in existing requirements or the adoption of new requirements or policies, or if we are not able to maintain regulatory compliance, we may lose any marketing approval that we may have obtained.
47
Regulatory approval is limited by the FDA to those specific indications and conditions for which clinical safety and efficacy have been demonstrated, and we may be subject to fines, penalties or injunctions if we are determined to be promoting the use of our products for unapproved or “off-label” uses, resulting in damage to our reputation and business.
When the FDA or comparable foreign regulatory authorities issue regulatory approval for a product candidate, the regulatory approval is limited to those specific indications for which a product is approved. For example, the FDA approved KORSUVA injection for the treatment of moderate-to-severe CKD-AP in adults undergoing hemodialysis indication. If we are not able to obtain FDA approval for any desired future indications for our products and product candidates, our ability to effectively market and sell our products may be reduced and our business may be adversely affected.
While physicians may choose to prescribe drugs for uses that are not described in the product’s labeling and for uses that differ from those tested in clinical studies and approved by the regulatory authorities, we are prohibited from marketing and promoting the products for indications that are not specifically approved by the FDA. These “off-label” uses are common across medical specialties and may constitute an appropriate treatment for some patients in varied circumstances. Regulatory authorities in the United States generally do not restrict or regulate the behavior of physicians in their choice of treatment within the practice of medicine. Regulatory authorities do, however, restrict communications by pharmaceutical companies on off-label use. If the FDA determines that our or our commercial partners’ promotional activities constitute promotion of an off-label use, it could request that we modify our promotional materials. Further, off-label promotion could subject us to regulatory or enforcement actions by the FDA and other agencies, including issuance of warning letters or untitled letters, suspension or withdraw an approved product from the market, mandatory or voluntary recalls, civil fines, disgorgement of money, operating restrictions, additional reporting requirements and/or oversight if we become subject to a corporate integrity agreement or similar agreement, injunctions or criminal prosecution, any of which could significantly harm our business.
Failure to obtain marketing approval in international jurisdictions would prevent our product candidates from being marketed abroad.
In order to market and sell our products in the EU and many other jurisdictions, we or our collaborators or partners must obtain separate marketing approvals and comply with numerous and varying regulatory requirements. For example, our partner, VFMCRP, submitted an MAA to the EMA in March 2021, which was accepted for review by the EMA. Although we obtained FDA approval of KORSUVA injection in the U.S., the approval procedure varies among countries and can involve additional testing. The time required to obtain approval may differ substantially from that required to obtain FDA approval. The regulatory approval process outside the United States generally includes all of the risks associated with obtaining FDA approval. In addition, in many countries outside the United States, it is required that the product be approved for reimbursement before the product can be approved for sale in that country. We or these third parties may not obtain approvals from regulatory authorities outside the United States on a timely basis, if at all. Approval by the FDA does not ensure approval by regulatory authorities in other countries or jurisdictions, and approval by one regulatory authority outside the United States does not ensure approval by regulatory authorities in other countries or jurisdictions or by the FDA. However, the failure to obtain approval in one jurisdiction may compromise our or our collaborators’ or partners’ ability to obtain approval elsewhere. We or our collaborators or partners may not be able to file for marketing approvals and may not receive necessary approvals to commercialize our products in any market.
Our products, including KORSUVA injection, may have undesirable side effects that may require them to be taken off the market, require them to include safety warnings or otherwise limit their sales. Further, our product candidates may have serious adverse events or undesirable side effects that may limit dosing in development, delay or prevent regulatory or marketing approval.
Undesirable side effects caused by our product candidates could cause us or regulatory authorities to limit dosage in development or interrupt, delay or halt clinical trials and could result in a more restrictive label or the delay or denial of regulatory approval by the FDA or other comparable foreign authorities. For example, in February 2016, the FDA placed our adaptive trial of I.V. difelikefalin for postoperative pain on IND clinical hold pending a safety review. The
48
clinical hold was based on a stopping rule related to elevated serum sodium levels of greater than 150 mmol/L. After the safety review was completed, the FDA removed this clinical hold in April 2016 and the clinical trial was resumed in June 2016. If other concerns are raised regarding the safety of a new drug as a result of undesirable side effects identified during clinical testing, the FDA may order us to cease further development, decline to approve the drug or issue a letter requesting additional data or information prior to making a final decision regarding whether or not to approve the drug. The number of such requests for additional data or information issued by the FDA in recent years has increased and resulted in substantial delays in the approval of several new drugs. Undesirable side effects caused by I.V. difelikefalin or any of our other current or future product candidates could also result in denial of regulatory approval by the FDA or other regulatory authorities for any or all targeted indications or the inclusion of unfavorable information in our product labeling, and in turn prevent us from commercializing and generating revenues from the sale of I.V. difelikefalin for acute post-operative pain or any other product candidate. Approval of our current or future product candidates may include aspects of product labeling that limit its commercial use, including a Boxed Warning, REMS or other limitations of use.
To date, the side effects observed in the completed I.V. difelikefalin clinical trials include dizziness, transient facial tingling, a state of near-sleep, or somnolence, and hypernatremia, an electrolyte disturbance that is defined by an elevated sodium level in the blood, which we believe is secondary, at least in part, to another side effect, aquaresis, that is defined as electrolyte-free urination. As described above, the observation of mild to moderate hypernatremia in our adaptive trial for postoperative pain triggered a stopping rule in the trial protocol and led the FDA to institute an IND clinical hold related to the trial, pending a safety review. Prolonged aquaresis can result in a negative fluid balance if the excreted water is not replaced by oral or intravenous fluids, and although we recommend steps to control fluid balance, we cannot be certain that such instructions will be followed by healthcare providers and/or patients, and failure to follow such instructions may be accompanied by adverse events associated with negative fluid balance, including disability and death. We believe that one such adverse event, which has been observed, postural tachycardia, an elevation of heart rate upon standing up, is a physiological reflex that can be triggered as a result of decreased intravascular volume caused by a negative fluid balance. We have observed transient prolactin elevations, which are brief increases in the concentration of the hormone prolactin in the bloodstream, in response to I.V. difelikefalin, which we have measured as a nonselective opioid biomarker since both kappa and mu opioids elicit this effect. We cannot be certain that such elevations in prolactin will be transient, safe, and well tolerated in all patients. In addition, previously developed kappa opioid agonists, the pharmacological class of drugs that difelikefalin belongs to, have been associated with poorly tolerated psychiatric side effects, such as a feeling of emotional and mental discomfort, or dysphoria, and hallucinations, at high doses, particularly for prior generations of kappa opioid agonists with substantially unrestricted or only partially restricted entry to the CNS. Although we have not observed psychiatric side effects in any difelikefalin clinical trials to date, we cannot be certain that these side effects or others will not be observed in the future, or that the FDA will not require additional trials or impose more severe labeling restrictions due to these side effects or other concerns. The drug-related side effects could affect patient recruitment or the ability of enrolled patients to complete the trial or result in potential product liability claims. Any of these occurrences may harm our business, financial condition and prospects significantly.
Additionally, our products, including KORSUVA injection, are subject to continuing regulatory oversight. Drugs are more widely used by patients once approval has been obtained and therefore side effects and other problems may be observed after approval that were not seen or anticipated, or were not as prevalent or severe, during pre-approval clinical trials or nonclinical studies. The subsequent delivery of previously unknown problems with a product, or public speculation about adverse safety events, could face a number of potentially significant negative consequences could result, including:
| ● | regulatory authorities may suspend or withdraw approvals of such product; |
| ● | regulatory authorities may require additional warnings on the label; |
| ● | we may be required to create a medication guide outlining the risks of such side effects for distribution to patients; |
| ● | issue warning letters; |
49
| ● | mandate modifications to promotional materials or require us to provide corrective information to healthcare practitioners; |
| ● | require us or our collaborators to enter into a consent decree, which can include imposition of various fines, reimbursements for inspection costs, required due dates for specific actions and penalties for noncompliance; |
| ● | impose other civil or criminal penalties; |
| ● | impose restrictions on operations, including costly new manufacturing requirements; |
| ● | seize or detain products or require a product recall; |
| ● | we could be sued and held liable for harm caused to patients; |
| ● | the sales of the product may decrease significantly; and |
| ● | our reputation may suffer. |
Any of these events could prevent us from achieving or maintaining market acceptance of KORSUVA injection and the particular product candidate, if approved, and could significantly harm our business, results of operations and prospects.
If we experience continuous delays or difficulties in the enrollment of patients in clinical trials, our receipt of necessary regulatory approvals could be delayed or prevented.
We may not be able to initiate or continue conducting clinical trials for our product candidates if we are unable to locate and enroll a sufficient number of eligible patients to participate in these trials as required by the FDA or similar regulatory authorities outside the United States. Some of our competitors have ongoing clinical trials for product candidates that treat the same indications as our product candidates, and patients who would otherwise be eligible for our clinical trials may instead enroll in clinical trials of our competitors’ product candidates. Patient enrollment is affected by other factors including:
| ● | the size and nature of the patient population; |
| ● | the severity of the disease under investigation; |
| ● | the eligibility criteria for, and design of, the trial in question; |
| ● | the perceived risks and benefits of the product candidate under study; |
| ● | competition in recruiting and enrolling patients in clinical trials; |
| ● | the efforts to facilitate timely enrollment in clinical trials; |
| ● | the patient referral practices of physicians; |
| ● | the ability to monitor patients adequately during and after treatment; |
| ● | the proximity and availability of clinical trial sites for prospective patients; and |
| ● | delays or difficulties due to the ongoing COVID-19 pandemic. |
50
For example, we experienced a delay in patient enrollment for our Phase 2 clinical trial of Oral KORSUVA (difelikefalin) for the treatment of pruritus in patients with hepatic impairment due to PBC, and could in the future experience delays in either of our ongoing Phase 2 clinical trials as patient enrollment in both of these trials is not yet complete.
Our inability to enroll a sufficient number of patients for our clinical trials would result in significant delays and could require us to abandon one or more clinical trials altogether. We may encounter difficulties and/or delays in completing our planned enrollments. Enrollment delays in our clinical trials may result in increased development costs for our product candidates, or the inability to complete development of our product candidates, which would cause the value of our company to decline, limit our ability to obtain additional financing, and materially impair our ability to generate revenues.
Risks Related to Our Financial Condition and Capital Requirements
We have incurred significant losses from our inception, and although we generated net income in 2020, we anticipate that we may incur losses in the foreseeable future. Our first commercial product was only recently approved, and we may never maintain profitability.
We are an early commercial-stage biopharmaceutical company. For the last several years, we have focused our efforts primarily on developing KORSUVA injection and Oral KORSUVA (difelikefalin) with the goal of achieving regulatory approval and in August 2021, the FDA approved KORSUVA injection for the treatment of moderate-to-severe CKD-aP in adults undergoing hemodialysis. Since inception, we have incurred significant operating and net losses. We incurred net losses of $88.4 million and $106.4 million for the years ended December 31, 2021 and 2019, respectively. As of December 31, 2021, we had an accumulated deficit of $480.8 million. Although we generated net income for the year ended December 31, 2020 as a result of a commercial license transaction, we expect to continue to incur significant expenses and operating and net losses in the foreseeable future, as we continue to prepare for the commercialization of KORSUVA injection and develop and seek marketing approval for our product candidates. Our financial results may fluctuate significantly from year to year, depending on the timing of our clinical trials, the receipt of additional milestone payments, if any, under our agreements with Vifor, VFMCRP, Maruishi and CKDP, the receipt of payments under any future agreements we may enter into, and our expenditures on other R&D activities as well as any payments owed under the License Agreement with Enteris and any future similar agreements.
In addition, we expect to incur significant sales, marketing and manufacturing expenses related to our product candidates, if they are approved by the FDA, and expenses related to the commercialization of KORSUVA injection. As a result, we expect to continue to incur significant losses for the foreseeable future as we:
| ● | continue the development of Oral KORSUVA (difelikefalin) for AD-aP, NDD-CKD, CLD-PBC and NP; |
| ● | seek regulatory approvals for any other product candidate that successfully completes clinical trials; |
| ● | establish a sales, marketing and distribution infrastructure and scale up external manufacturing capabilities to commercialize any other products for which we may obtain regulatory approval; |
| ● | maintain, expand and protect our global intellectual property portfolio; |
| ● | hire additional clinical, quality control and scientific personnel; and |
| ● | add operational, financial and management information systems and personnel, including personnel to support our drug development and potential future commercialization efforts. |
To become and remain profitable from product sales, we must succeed in developing and eventually commercializing one or more products that generate significant revenue. For example, revenues from KORSUVA injection may not be sufficient to enable us to reach profitability. In order to commercialize any additional product
51
candidates, we will need to be successful in a range of challenging activities, including successful registration of Oral KORSUVA (difelikefalin), discovering additional product candidates and completing preclinical testing and clinical trials for those product candidates, potentially entering into collaboration and license agreements, obtaining regulatory approval for product candidates and manufacturing, marketing and selling approved products and product candidates for which we may obtain regulatory approval. We may never succeed in these activities and, even if we do, may never achieve profitability.
Because of the numerous risks and uncertainties associated with pharmaceutical product development, we are unable to accurately predict the timing or amount of increased expenses or when, or if, we will be able to achieve profitability. If we are required by the FDA or foreign regulatory authorities, to perform studies in addition to those currently expected, or if there are any delays in completing our clinical trials or the development of any of our product candidates, our expenses could increase.
Even if we do achieve profitability from product sales, we may not be able to sustain or increase profitability on a quarterly or annual basis. Our failure to become and remain profitable would depress the value of our company and could impair our ability to raise capital, expand our business, maintain our R&D efforts, diversify our product offerings or even continue our operations. A decline in the value of our company could also cause you to lose all or part of your investment.
Our operating history makes it difficult to evaluate our business and prospects.
We commenced operations in 2004, and our operations to date have been limited to organizing and staffing our company, business planning, raising capital and advancing our products and product candidates, including KORSUVA injection and Oral KORSUVA (difelikefalin), through clinical development. We have not yet demonstrated an ability to successfully commercialize a product. With the approval of KORSUVA injection, we will need to expand our capabilities to support commercial activities of our commercial partners. We may not be successful in adding such capabilities. Consequently, any predictions about our future performance may not be as accurate as they could be if we had a history of successfully developing and commercializing pharmaceutical products.
We may need additional funding and may be unable to raise capital when needed, which would force us to delay, reduce or eliminate our product development programs or commercialization efforts.
Conducting clinical trials, pursuing regulatory approvals, establishing outsourced manufacturing relationships and successfully manufacturing and commercializing our products and product candidates is expensive. We may need to raise additional capital to:
| ● | fund our operations and continue our efforts to hire additional personnel for the commercialization of KORSUVA injection; |
| ● | qualify and outsource the commercial-scale manufacturing of our products, including KORSUVA injection, under cGMP; |
| ● | continue the further development of Oral KORSUVA (difelikefalin) for AD-aP, NDD-CKD, CLD-PBC and NP; and |
| ● | in-license other product candidates. |
As of December 31, 2021, we believe that with our current unrestricted cash and cash equivalents and available-for-sale marketable securities will be sufficient to fund our currently anticipated operating expenses and capital requirements through 2023, without giving effect to any additional potential milestone payments or potential product revenue we may receive under our licensing and collaboration agreements with Vifor, VFMCRP, Maruisihi and CKDP. We have based this estimate on assumptions that may prove to be wrong and we could spend our available financial resources faster than we currently expect. Further, because we do not have sufficient financial resources to meet all of
52
our development objectives, in particular the completion of our development of Oral KORSUVA (difelikefalin) for the treatment of AD-aP, NDD-CKD, CLD-PBC and NP, we will need to raise additional capital. If we are not able to do so, we could be required to postpone, scale back or eliminate some, or all, of these objectives. Our future funding requirements will depend on many factors, including, but not limited to:
| ● | the success of the commercialization of KORSUVA injection and any current and future product candidates; |
| ● | the cost and timing of manufacturing sufficient supplies of KORSUVA injection for commercialization; |
| ● | the rate of progress and costs related to Phase 2 and Phase 3 development of Oral KORSUVA (difelikefalin) for our product candidates and other indications; |
| ● | the rate of progress and costs for the submission and review of an NDA for any product candidates that we may in-license or acquire in the future, and the potential that we may need to conduct additional clinical trials to support applications for regulatory approval; |
| ● | the costs of filing, prosecuting, defending and enforcing any patent claims and other intellectual property rights associated with our product candidates, including any such costs we may be required to expend if our licensors are unwilling or unable to do so; |
| ● | the effect of competing technological and market developments; and |
| ● | the terms and timing of any collaborative, licensing, co-promotion or other arrangements that we may establish. |
Future capital requirements will also depend on the extent to which we acquire or invest in additional complementary businesses, products and technologies. Until we can generate a sufficient amount of product revenue, if ever, we expect to finance future cash needs through public or private equity offerings, debt financings, milestone and royalty payments from corporate collaboration and licensing arrangements, as well as through interest income earned on cash and investment balances. We cannot be certain that additional funding will be available on acceptable terms, or at all, and our ability to raise additional capital may be adversely impacted by potential worsening global economic conditions and the continuing disruptions to and volatility in the credit and financial markets in the United States and worldwide resulting from the ongoing COVID-19 pandemic. If adequate funds are not available, we may be required to delay, reduce the scope of, or eliminate, one or more of our development programs or our commercialization efforts.
Risks Related to Our Dependence on Third Parties
We are dependent on third parties to decide to utilize KORSUVA injection and to make it readily available at the point of care throughout their dialysis centers or hospitals.
In addition to extensive internal efforts, the successful commercialization of KORSUVA injection will require many third parties, over whom we have no control, to decide to utilize KORSUVA injection and to make it readily available at the point of care throughout their hospitals. These third parties include physicians, dialysis providers, pharmacists and hospital pharmacy and therapeutics committees, which are commonly referred to as P&T committees. Generally, before we can attempt to sell KORSUVA injection in a hospital or dialysis center, it must be approved for addition to that hospital or dialysis center’s list of approved drugs, or formulary list, by the institution’s P&T committee. An institutional P&T committee typically governs all matters pertaining to the use of medications within the institution, including review of medication formulary data and recommendations for the appropriate use of drugs within the institution to the medical staff. The frequency of P&T committee meetings at various institutions varies considerably, and P&T committees often require additional information to aid in their decision-making process, so we may experience substantial delays in obtaining formulary approvals. Additionally, institutions may be concerned that the cost of acquiring KORSUVA injection for use in their institutions will adversely impact their overall pharmacy budgets, which could cause institution staff to resist efforts to add KORSUVA injection to the formulary, or to implement restrictions on the usage of the drug in order to control costs, either initially or later, when the increasing use of KORSUVA injection
53
within their institution begins to significantly impact their budgets. We cannot guarantee that we will be successful in getting the approvals we need from enough P&T committees and overcoming any financial objections raised by institution staff quickly enough to maintain and grow institutional sales of KORSUVA injection.
We rely on third parties to perform many essential services for KORSUVA injection and may do so in the future for any products that we commercialize, including services related to warehousing and inventory control, distribution, customer service, accounts receivable management, cash collection and adverse event reporting. If these third parties fail to perform as expected or to comply with legal and regulatory requirements, our ability to commercialize KORSUVA injection or any other product candidate, will be significantly impacted and we may be subject to regulatory sanctions.
We retain third-party service providers to perform a variety of functions related to the sale and distribution of KORSUVA injection and may do so in the future for our other current or future product candidates, key aspects of which will be out of our direct control. These service providers provide key services related to warehousing and inventory control, distribution, customer service, accounts receivable management and cash collection, and, as a result, most of our inventory are stored at a single warehouse maintained by one such service provider. Thus, we substantially rely on it as well as other third-party providers that perform services for us, including entrusting our inventories of products to their care and handling. If these third-party service providers fail to comply with applicable laws and regulations, fail to meet expected deadlines, or otherwise do not carry out their contractual duties to us, or encounter physical or natural damage at their facilities, our ability to deliver product to meet commercial demand would be significantly impaired. In addition, we have engaged third parties to perform various other services for us relating to adverse event reporting, safety database management, fulfillment of requests for medical information regarding our product candidates and related services. If the quality or accuracy of the data maintained by these service providers is insufficient, or these third parties otherwise fail to comply with regulatory requirements related to adverse event reporting, we could be subject to regulatory sanctions.
We are dependent on our collaboration agreements for certain revenues, and if our commercial partners do not perform their obligations under such agreements, we could lose revenues.
In October 2020, we entered into a license agreement with Vifor under which we granted Vifor an exclusive license solely in the United States to use, distribute, offer for sale, promote, sell and otherwise commercialize our product candidate KORSUVA (difelikefalin) injection for all therapeutic uses relating to the inhibition, prevention or treatment of itch associated with pruritus in hemodialysis and peritoneal dialysis patients in the United States. In May 2018, we entered into an agreement with VFMCRP under which we granted VFMCRP a license to seek regulatory approval to commercialize, import, export, use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA (difelikefalin) injection for all therapeutic uses to prevent, inhibit or treat itch associated with pruritus in hemodialysis and peritoneal-dialysis patients worldwide (excluding the United States, Japan and South Korea). In April 2013, we entered into an agreement with Maruishi under which we granted Maruishi an exclusive license to develop, manufacture and commercialize products containing difelikefalin in Japan. Also, in April 2012, we entered into an agreement with CKDP under which we granted CKDP an exclusive license to develop, manufacture and commercialize products containing difelikefalin in South Korea. Under the VFMCRP Agreement, we are responsible, at our own cost, to undertake clinical and non-clinical development. We are also responsible to provide all content and subject matter expertise required for registration with the EMA in the EU that will be needed by VFMCRP for such registration, including participation in regulatory meetings, as needed. VFMCRP will contribute, at its own cost, its clinical development expertise as reasonably useful for such development activities, such as preparing the clinical results that we present to it in a format acceptable to the EMA to obtain marketing approval in the EU. Maruishi and CKDP are required to use commercially reasonable efforts, at their expense, to develop, obtain regulatory approval for and commercialize difelikefalin in Japan and South Korea, respectively. Our receipt of milestone payments and royalties under these agreements is dependent on the continued efforts by Vifor, VFMCRP, Maruishi and CKDP, respectively, and their failure to adequately develop or commercialize the licensed products, or any default or inability to meet their payment obligations under their respective agreements, could harm our revenues and business.
54
Any collaboration arrangements that we are a party to, such as our collaboration with Vifor Pharma, or may enter into in the future may not be successful, which could adversely affect our ability to develop and commercialize our product candidates.
Our business model is to commercialize our product and product candidates in the United States and generally to seek collaboration arrangements with pharmaceutical or biotechnology companies for the development or commercialization of our product candidates in the rest of the world. We currently have license agreements with Vifor and VFMCRP (KORSUVA injection for CKD-aP in dialysis patients) as well as Maruishi and CKDP (difelikefalin - both I.V. and Oral). In addition to our existing agreements, we may enter into additional collaboration arrangements in the future on a selective basis. Our existing collaborations and future collaboration arrangements may not be successful. The success of our existing and future collaboration arrangements will depend heavily on the efforts and activities of our collaborators.
Collaborators generally have significant discretion in determining the efforts and resources that they will apply to these collaboration arrangements. Disagreements between parties to a collaboration arrangement regarding clinical development and commercialization matters can lead to delays in the development process or commercializing the applicable product candidate and, in some cases, termination of the collaboration arrangement. These disagreements can be difficult to resolve if neither of the parties has final decision-making authority.
Collaborations with pharmaceutical companies and other third parties often are terminated or allowed to expire by the other party. For example, the Vifor, VFMCRP, Maruishi and CKDP Agreements may be terminated by our collaborator for our breach or insolvency, each of Vifor and VFMCRP may terminate its respective agreement (in its entirety or with respect to any countries within the Territory upon written notice to us) upon the earlier of (1) acceptance for filing of an NDA covering Licensed Product filed with the FDA (after completion of the Phase 3 program) or (2) the third anniversary of the Effective Date. Maruishi may terminate its agreement with us at will, and CKDP may terminate its agreement with us in certain circumstances relating to patent invalidity or unenforceability or generic entry by a third party, as further described in the section titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations - Collaboration and License Agreements” above. Any such termination or expiration would adversely affect us financially and could harm our business reputation. Our current collaborations and any future collaborations we might enter into may pose a number of risks, including the following:
| ● | collaborators may not perform their obligations as expected; |
| ● | collaborators may not pursue development and commercialization of our products or any product candidates that achieve regulatory approval or may elect not to continue or renew development or commercialization programs based on clinical trial results, changes in the collaborators’ strategic focus or available funding that divert resources or create competing priorities; |
| ● | collaborators may delay clinical trials, provide insufficient funding for a clinical trial program, stop a clinical trial or abandon a product candidate, repeat or conduct new clinical trials or require a new formulation of a product candidate for clinical testing; |
| ● | collaborators could fail to make timely regulatory submissions for a product or product candidate; |
| ● | collaborators may not comply with all applicable regulatory requirements or may fail to report safety data in accordance with all applicable regulatory requirements; |
| ● | collaborators could independently develop, or develop with third parties, products that compete directly or indirectly with our products or product candidates if the collaborators believe that competitive products are more likely to be successfully developed or can be commercialized under terms that are more economically attractive than ours; |
55
| ● | product candidates discovered in collaboration with us may be viewed by our collaborators as competitive with their own product candidates or products, which may cause collaborators to cease to devote resources to the commercialization of our product candidates; |
| ● | a collaborator with marketing and distribution rights to one or more of our products or product candidates that achieve regulatory approval may not commit sufficient resources to the marketing and distribution of such product or products; |
| ● | disagreements with collaborators, including disagreements over proprietary rights, contract interpretation or the preferred course of development, might cause delays or termination of the research, development or commercialization of products and product candidates, might lead to additional responsibilities for us with respect to products and product candidates, or might result in litigation or arbitration, any of which would be time-consuming and expensive; |
| ● | collaborators may not properly maintain or defend our intellectual property rights or may use our proprietary information in such a way as to invite litigation that could jeopardize or invalidate our intellectual property or proprietary information or expose us to potential litigation; |
| ● | collaborators may infringe the intellectual property rights of third parties, which may expose us to litigation and potential liability; and |
| ● | collaborations, including our collaboration with Maruishi, may be terminated for the convenience of the collaborator and, if terminated, we could be required to raise additional capital to pursue further development or commercialization of the applicable product candidates. |
Additionally, collaborators may elect not to pursue, or pursue as vigorously, the development or commercialization of our product or product candidates as a result of external factors, such as an acquisition or merger. For example, Vifor recently entered into a merger agreement with CSL Limited, a global specialty pharmaceutical company, pursuant to which CSL Limited would acquire all publicly held Vifor Pharma shares if such transaction is completed. When biopharma companies are acquired, it is not uncommon for the acquiring company to have a different strategic focus and priorities than those of the acquired company, which could lead to different decisions with respect to product commercialization efforts. Accordingly, if the acquisition is consummated, CSL Limited may choose not to prioritize KORSUVA injection to the same extent as Vifor Pharma would as a standalone company. If this were to occur, it is possible that the commercialization of KORSUVA injection could suffer, which would have a material adverse impact on our business and results of operations.
If our current collaborations or any other collaborations we might enter into in the future do not result in the successful development and commercialization of products or if one of our collaborators terminates its agreement with us, we may not receive any future research funding or milestone or royalty payments under the collaboration. If we do not receive the funding we expect under these agreements, our development of our product candidates could be delayed and we may need additional resources to develop our product candidates and our product platform. All of the risks relating to our product development, regulatory approval and commercialization described in this Annual Report on Form 10-K also apply to the activities of our collaborators in their respective jurisdictions.
Additionally, if any current or future collaborator of ours is involved in a business combination, the collaborator might deemphasize or terminate development or commercialization of any product candidate licensed to it by us. If one of our collaborators terminates its agreement with us, we may find it more difficult to attract new collaborators and our reputation in the business and financial communities could be adversely affected.
For KORSUVA injection and any other current or future product candidates, we may in the future determine to collaborate with additional pharmaceutical and biotechnology companies for their development and potential commercialization. We face significant competition in seeking appropriate collaborators. Our ability to reach a definitive agreement for collaboration will depend, among other things, upon our assessment of the collaborator’s resources and
56
expertise, the terms and conditions of the proposed collaboration and the proposed collaborator’s evaluation of a number of factors. If we are unable to reach agreements with suitable collaborators on a timely basis, on acceptable terms, or at all, we may have to curtail the development of a product candidate, reduce or delay its development program or one or more of our other development programs, delay its potential commercialization or reduce the scope of any sales or marketing activities, or increase our expenditures and undertake development or commercialization activities at our own expense. If we elect to fund and undertake development or commercialization activities on our own, we may need to obtain additional expertise and additional capital, which may not be available to us on acceptable terms or at all. If we fail to enter into collaborations and do not have sufficient funds or expertise to undertake the necessary development and commercialization activities, we may not be able to further develop our product candidates or bring them to market or continue to develop our product platform or successfully commercialize our products and our business may be materially and adversely affected.
Risks Related to Legal and Compliance Matters
If we fail to comply with federal and state healthcare laws, including fraud and abuse, and transparency laws, we could face substantial penalties and our business, results of operations, financial condition and prospects could be adversely affected.
As a pharmaceutical company, even though we do not and will not control referrals of healthcare services or bill directly to Medicare, Medicaid or other third-party payers, certain federal and state healthcare laws and regulations pertaining to fraud and abuse, transparency and patients’ rights may be applicable to our business. The healthcare laws and regulations that may affect our ability, and our partners’ and collaborators’ ability, to operate include, but are not limited to:
| ● | the federal Anti-Kickback Statute, which regulates, among other things, our marketing practices, educational programs, pricing policies, and relationships with healthcare providers or other entities, by prohibiting, among other things, any person or entity from knowingly and willfully soliciting, receiving, offering or paying any remuneration, directly or indirectly, overtly or covertly, in cash or in kind, to induce, or in return for, the purchase, recommendation, lease, order or furnishing of an item or service reimbursable, in whole or in part, under a federal healthcare program, such as the Medicare and Medicaid programs; |
| ● | federal civil and criminal false claims laws, including without limitation the federal civil False Claims Act, and civil monetary penalties law, which prohibit, among other things, individuals or entities from knowingly presenting, or causing to be presented, false or fraudulent claims for payment or approval from a federal health care program (including Medicare and Medicaid); |
| ● | Federal Health Insurance Portability and Accountability Act of 1996, or HIPAA, which created additional federal criminal statutes that prohibit, among other things, knowingly and willfully executing, or attempting to execute, a scheme to defraud any healthcare benefit program or to obtain, by means of false or fraudulent pretenses, representations, or promises, any of the money or property owned by, or under the custody or control of, any health care benefit program, regardless of the payer (e.g., public or private) and knowingly and willfully falsifying, concealing, or covering up by any trick, scheme or device a material fact or making any materially false statements in connection with the delivery of, or payment for, health care benefits, items or services relating to healthcare matters; |
| ● | federal transparency laws, including the federal Physician Payments Sunshine Act, that requires certain manufacturers of drugs, devices, biologics, and medical supplies for which payment is available under Medicare, Medicaid, or the Children’s Health Insurance Program to report annually to CMS information related to payments and other transfers of value provided to physicians (defined to include doctors of medicine, dentists, optometrists, podiatrists and chiropractors), other healthcare professionals (such as physician assistants and nurse practitioners), and teaching hospitals, and applicable manufacturers and group purchasing organizations to report annually to CMS ownership and investment interests held by physicians and their immediate family members; |
57
| ● | state law equivalents of each of the above federal laws, such as anti-kickback and false claims laws which may apply to items or services reimbursed by any third-party payer, including commercial insurers; and |
| ● | state laws that require pharmaceutical companies to comply with the pharmaceutical industry’s voluntary compliance guidelines and the relevant compliance guidance promulgated by the federal government, or otherwise restrict payments that may be made to healthcare providers and other potential referral sources; state laws that require drug manufacturers to report information related to the pricing of certain drugs, as well as payments and other transfers of value to physicians and other healthcare providers or marketing expenditures; and state and local laws that require the registration of pharmaceutical sales representatives, many of which differ from each other in significant ways and may not have the same effect, thus complicating compliance efforts. |
Because of the breadth of these laws and the narrowness of the statutory exceptions and regulatory safe harbors available under these laws, it is possible that some of our business activities could be subject to challenge under one or more of such laws. Pharmaceutical and other healthcare companies continue to be prosecuted under the federal false claims laws for numerous activities, including those related to research, sales, marketing and promotional programs. In addition, recent health care reform legislation has strengthened these laws. For example, the Patient Protection and Affordable Care Act of 2010, as amended by the Health Care and Education Reconciliation Act of 2010, or the Health Care Reform Law, among other things, amends the intent requirement of the federal Anti-Kickback Statute and certain other criminal healthcare fraud statutes. As a result, a person or entity no longer needs to have actual knowledge of these statutes or specific intent to violate them in order to commit a violation. Moreover, the Health Care Reform Law provides that the government may assert that a claim including items or services resulting from a violation of the federal Anti-Kickback Statute constitutes a false or fraudulent claim for purposes of the federal civil False Claims Act. To the extent that any product we make is sold in a foreign country, we may be subject to similar foreign laws and regulations. If we or our operations are found to be in violation of any of the laws described above or any other governmental regulations that apply to us, we may be subject to significant penalties, including administrative, civil and criminal penalties, damages, fines, disgorgement, exclusion from participation in U.S. federal or state health care programs, contractual damages, reputational harm, imprisonment, diminished profits and future earnings, additional reporting requirements and/or oversight if we become subject to a corporate integrity agreement or similar agreement to resolve allegations of non-compliance with these laws, and the curtailment or restructuring of our operations, any of which could materially adversely affect our ability to operate our business and our financial results. Although an effective compliance program can mitigate the risk of investigation and prosecution for violations of these laws, the risks cannot be entirely eliminated. Any action against us for violation of these laws, even if we successfully defend against it, could cause us to incur significant legal expenses and divert our management’s attention from the operation of our business. Moreover, achieving and sustaining compliance with applicable federal and state transparency and fraud and abuse laws may prove costly. If any of the physicians or other healthcare providers or entities with whom we do business, including our partners or collaborators, is found not to be in compliance with applicable laws, it may be subject to significant criminal, civil or administrative sanctions, including but not limited to, exclusions from participation in government healthcare programs, which could also materially affect our business.
Changes in and failures to comply with applicable U.S. and foreign privacy and data protection laws, regulations and standards may subject us to liabilities and adversely affect our business, operations and financial performance.
We are subject to or affected by numerous federal, state and foreign laws and regulations, as well as regulatory guidance, governing the collection, use, disclosure, retention, and security of personal data, such as information that we collect about participants and healthcare providers in connection with clinical trials in the U.S. and abroad. The global data protection landscape is rapidly evolving, and implementation standards and enforcement practices are likely to remain uncertain for the foreseeable future. This evolution may create uncertainty in our business, affect our or our service providers’ ability to operate in certain jurisdictions or to collect, store, transfer use and share personal data, result in liability or impose additional costs on us. The cost of compliance with these laws, regulations and standards is high and is likely to increase in the future. Any failure or perceived failure by us to comply with federal, state, or foreign laws or self-regulatory standards could result in negative publicity, diversion of management time and effort and proceedings against us by governmental entities or others. In many jurisdictions, enforcement actions and consequences for noncompliance are rising.
58
In the U.S., HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act of 2009, or HITECH, imposes certain requirements relating to the privacy, security and transmission of individually identifiable health information without appropriate authorization by entities subject to the rule, including health plans, healthcare clearinghouses, certain healthcare providers, and their business associates and covered subcontractors that perform services for them that involve the creation, use, maintenance or disclosure of, individually identifiable health information. In the event we are subject to HIPAA and we or our covered subcontractors fail to properly maintain the privacy and security of certain individually identifiable health information, or we or our covered subcontractors are responsible for an inadvertent disclosure or security breach of such individually identifiable health information, we could be subject to enforcement measures, including civil and criminal penalties and fines for violations of state and federal privacy or security standards, such as HIPAA and HITECH, and their respective implementing regulations. Additionally, certain states have adopted comparable privacy and security laws and regulations, some of which may be more stringent than HIPAA. For example, on June 28, 2018, California enacted the California Consumer Privacy Act, or CCPA, which takes effect on January 1, 2020. The CCPA gives California residents expanded rights to access and delete their personal information, opt out of certain personal information sharing, and receive detailed information about how their personal information is used. The CCPA provides for civil penalties for violations, as well as a private right of action for data breaches that is expected to increase data breach litigation. The CCPA may increase our compliance costs and potential liability. Some observers have noted that the CCPA could mark the beginning of a trend toward more stringent privacy legislation in the U.S., such as similar privacy legislation in Virginia and in Colorado, which could increase our potential liability and adversely affect our business.
Our operations abroad may also be subject to increased scrutiny or attention from data protection authorities. Many countries in these regions have established or are in the process of establishing privacy and data security legal frameworks with which we or our partners, collaborators, customers, or service providers must comply. For example, the EU has adopted the General Data Protection Regulation, or GDPR, which went into effect in May 2018 and introduced strict requirements for processing personal data. The GDPR is likely to increase compliance burden on us, including by mandating potentially burdensome documentation requirements and granting certain rights to individuals to control how we collect, use, disclose, retain and leverage information about them or how we obtain consent from them. The processing of sensitive personal data, such as physical health condition, may impose heightened compliance burdens under the GDPR and is a topic of active interest among foreign regulators and supervisory bodies involved in the review and approval of clinical trials. In addition, the GDPR provides for breach reporting requirements, more robust regulatory enforcement and fines of up to 20 million euros or up to 4% of the annual global revenue. As we continue to expand into other foreign countries and jurisdictions, we may be subject to additional laws and regulations that may affect how we conduct business.
U.S. and foreign data protection laws, regulations and standards are subject to interpretation by various courts and other governmental authorities, thus creating potentially complex compliance issues for us and our future customers and strategic partners. Any liability from failure to comply with the requirements of these laws, to the extent such requirements are deemed to apply to our operations, could adversely affect our financial condition. The costs of complying with privacy and security related legal and regulatory requirements are burdensome and could have a material adverse effect on our results of operations.
If the government or other third-party payers fail to provide coverage and adequate reimbursement and payment rates for KORSUVA injection or any of our other current or future product candidates, if any, or if providers choose to use therapies that are less expensive, our revenue and prospects for profitability will be limited.
In both domestic and foreign markets, sales of KORSUVA injection and our future products (if approved) will depend in part upon the availability of coverage and reimbursement from third-party payers. Such third-party payers include government health programs such as Medicare and Medicaid, managed care providers, private health insurers and other organizations. Coverage decisions may depend upon clinical and economic standards that disfavor new drug products when more established or lower cost therapeutic alternatives are already available or subsequently become available. Assuming coverage is approved, the resulting reimbursement payment rates might not be adequate. KORSUVA injection for the treatment of pruritus in hemodialysis patients is expected to be designated as a component of the government’s bundled reimbursement for end stage renal disease treatment.
59
Our U.S. commercial partner, Vifor Pharma Group, submitted the payment reimbursement application for TDAPA and HCPCS to CMS in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years.
Additionally, many U.S. hospitals receive a fixed reimbursement amount per procedure for certain surgeries and other treatment therapies they perform, or a pre-determined rate for all hospital inpatient care provided as payment in full. Because, in these instances, the amount of reimbursement that such providers receive may not be based on the actual expenses the provider incurs, providers may choose to use therapies which are less expensive when compared to our product candidates. Accordingly, KORSUVA injection or any of our other current or future product candidates, if approved, will face competition from other therapies and drugs for these limited provider financial resources. We may need to conduct post-marketing studies in order to demonstrate the cost-effectiveness of any future products to the satisfaction of hospitals, other target customers and their third-party payers. Such studies might require us to commit a significant amount of management time and financial and other resources. Our future products might not ultimately be considered cost-effective. Third-party coverage and adequate reimbursement might not be available to enable us to maintain price levels sufficient to realize an appropriate return on investment in product development.
Third-party payers, whether foreign or domestic, or governmental or commercial, are developing increasingly sophisticated methods of controlling healthcare costs. In addition, in the United States, no uniform policy of coverage and reimbursement for drug products exists among third-party payers. Therefore, coverage and reimbursement for drug products can differ significantly from payer to payer. Further, we believe that future coverage and reimbursement will likely be subject to increased restrictions both in the United States and in international markets. Third-party coverage and reimbursement for our products or product candidates for which we receive regulatory approval may not be available or adequate in either the United States or international markets, which could have a negative effect on our business, results of operations, financial condition and prospects.
We are subject to recent legislation, regulatory proposals and healthcare payer initiatives that may increase our costs of compliance and adversely affect our ability to market our products, obtain collaborators and raise capital.
In March 2010, President Obama signed the Health Care Reform Law, which includes provisions that have changed, and likely will continue to change, health care financing and the delivery of health care in the United States. Among the provisions of the Health Care Reform Law of importance to the pharmaceutical industry are the following:
| ● | an annual, nondeductible fee on any entity that manufactures or imports certain branded prescription drugs and biologic agents, apportioned among these entities according to their market share in certain government healthcare programs; |
| ● | an increase in the statutory minimum rebates a manufacturer must pay under the Medicaid Drug Rebate Program to 23.1% and 13% of the average manufacturer price for most branded and generic drugs, respectively; |
| ● | a new methodology by which rebates owed by manufacturers under the Medicaid Drug Rebate Program are calculated for drugs that are inhaled, infused, instilled, implanted or injected; |
| ● | a new Medicare Part D coverage gap discount program, in which manufacturers must now agree to offer 70% point-of-sale discounts off negotiated prices of applicable brand drugs to eligible beneficiaries during their coverage gap period, as a condition for the manufacturer’s outpatient drugs to be covered under Medicare Part D; |
| ● | extension of manufacturers’ Medicaid rebate liability to covered drugs dispensed to individuals who are enrolled in Medicaid managed care organizations; |
| ● | expansion of eligibility criteria for Medicaid programs by, among other things, allowing states to offer Medicaid coverage to additional individuals with income at or below 133% of the Federal Poverty Level, thereby potentially increasing both the volume of sales and manufacturers’ Medicaid rebate liability; |
60
| ● | expansion of the entities eligible for discounts under the Public Health Service pharmaceutical pricing program; |
| ● | new transparency requirements under the federal Physician Payments Sunshine Act; |
| ● | a new requirement to annually report certain drug samples that manufacturers and distributors provide to licensed practitioners, or to pharmacies of hospitals or other healthcare entities; |
| ● | a licensure framework for follow-on biologic products; |
| ● | a new Patient-Centered Outcomes Research Institute to oversee, identify priorities in, and conduct comparative clinical effectiveness research, along with funding for such research; |
| ● | establishment of a Center for Medicare & Medicaid Innovation at the CMS to test innovative payment and service delivery models to lower Medicare and Medicaid spending, potentially including prescription drug spending; and |
| ● | expansion of healthcare fraud and abuse laws, including the federal civil False Claims Act and the federal Anti-Kickback Statute, new government investigative powers and enhanced penalties for non-compliance. |
There have been executive, judicial and Congressional challenges to certain aspects of the Health Care Reform Law. For example, on June 17, 2021 the U.S. Supreme Court dismissed a challenge on procedural grounds that argued the Health Care Reform Law is unconstitutional in its entirety because the “individual mandate” was repealed by Congress. Thus, the Health Care Reform Law will remain in effect in its current form. Further, prior to the Supreme Court ruling, on January 28, 2021, President Biden issued an executive order to initiate a special enrollment period for purposes of obtaining health insurance coverage through the Health Care Reform Law marketplace, which began on February 15, 2021 and remained open through August 15, 2021. The executive order also instructed certain governmental agencies to review and reconsider their existing policies and rules that limit access to healthcare, including among others, reexamining Medicaid demonstration projects and waiver programs that include work requirements, and policies that create unnecessary barriers to obtaining access to health insurance coverage through Medicaid or the Health Care Reform Law. It is also unclear how any such challenges and the healthcare reform measures of the Biden administration will impact the Health Care Reform Law and our business.
In addition, other legislative changes have been proposed and adopted since the Health Care Reform Law was enacted. These changes include, among other things, aggregate reductions to Medicare payments to providers of up to 2% per fiscal year, which went effective on April 1, 2013 and, following passage of the Bipartisan Budget Act of 2015, and subsequent legislative amendments, will remain in effect until 2031, except for a temporary suspension from May 1, 2020 through March 31, 2022 due to the COVID-19 pandemic, unless additional Congressional action is taken. Under current legislation, the actual reduction in Medicare payments will vary from 1% in 2022 to up to 3% in the final fiscal year of this sequester. In January 2013, President Obama signed into law the American Taxpayer Relief Act of 2012, which, among other things, further reduced Medicare payments to several providers and increased the statute of limitations period for the government to recover overpayments to providers from three to five years. Additionally, on March 11, 2021, President Biden signed the American Rescue Plan Act of 2021 into law, which eliminates the statutory Medicaid drug rebate cap, currently set at 100% of a drug’s average manufacturer price, for single source and innovator multiple source drugs, beginning January 1, 2024. Congress is considering additional health reform measures. These new laws may result in additional reductions in Medicare and other healthcare funding, which could have a material adverse effect on customers for our drugs, if approved, and, accordingly, our financial operations. Further, Congress is considering additional health reform measures.
We expect that the Health Care Reform Law, as well as other federal and state healthcare reform measures that may be adopted in the future, may result in more rigorous coverage criteria and in additional downward pressure on the price that we receive for KORSUVA injection or any approved product candidate. Any reduction in reimbursement from Medicare or other government healthcare programs may result in a similar reduction in payments from private payers. In addition, there have been several recent U.S. Presidential executive orders, Congressional inquiries and proposed and
61
enacted federal and state legislation designed to, among other things, bring more transparency to drug pricing, review the relationship between pricing and manufacturer patient programs, reduce the cost of drugs under Medicare, and reform government program reimbursement methodologies for drugs. At the federal level, the Trump administration used several means to propose or implement drug pricing reform, including through federal budget proposals, executive orders and policy initiatives. For example, on July 24, 2020 and September 13, 2020, the Trump administration announced several executive orders related to prescription drug pricing that seek to implement several of the administration’s proposals. As a result, the FDA concurrently released a final rule in September 2020, effective November 30, 2020, providing pathways for states to build and submit importation plans for drugs from Canada. Further, on November 20, 2020, the U.S. Department of Health and Human Services, or HHS, finalized a regulation removing safe harbor protection for price reductions from pharmaceutical manufacturers to plan sponsors under Part D, either directly or through pharmacy benefit managers, unless the price reduction is required by law. The implementation of the rule has been delayed by the Biden administration from January 1, 2022 to January 1, 2023 in response to ongoing litigation. The rule also creates a new safe harbor for price reductions reflected at the point-of-sale, as well as a safe harbor for certain fixed fee arrangements between pharmacy benefit managers and manufacturers, the implementation of which have also been delayed until January 1, 2023. On November 20, 2020, CMS issued an interim final rule implementing President Trump’s Most Favored Nation executive order, which would tie Medicare Part B payments for certain physician-administered drugs to the lowest price paid in other economically advanced countries. As a result of litigation challenging the Most Favored Nation model, on December 27, 2021, CMS published a final rule that rescinds the Most Favored Nation model interim final rule. Additionally, on March 11, 2021, President Biden signed the American Rescue Plan Act of 2021 into law, which eliminates the statutory Medicaid drug rebate cap, currently set at 100% of a drug’s average manufacturer price, for single source and innovator multiple source drugs, beginning January 1, 2024. Further, in July 2021, the Biden administration released an executive order that included multiple provisions aimed at prescription drugs. In response to Biden’s executive order, on September 9, 2021, HHS released a Comprehensive Plan for Addressing High Drug Prices that outlines principles for drug pricing reform. The plan sets out a variety of potential legislative policies that Congress could pursue as well as potential administrative actions HHS can take to advance these principles. No legislation or administrative actions have been finalized to implement these principles. At the state level, legislatures have increasingly passed legislation and implemented regulations designed to control pharmaceutical and biological product pricing, including price or patient reimbursement constraints, discounts, restrictions on certain product access and marketing cost disclosure and transparency measures, and, in some cases, to encourage importation from other countries and bulk purchasing. The implementation of cost containment measures or other healthcare reforms may prevent us from being able to generate revenue, attain profitability or commercialize our drugs.
Legislative and regulatory proposals have been made to expand post-approval requirements and restrict sales and promotional activities for drugs. We cannot be sure whether additional legislative changes will be enacted, or whether the FDA regulations, guidance or interpretations will be changed, or what the impact of such changes on the marketing approvals of our product candidates, if any, may be. In addition, increased scrutiny by the U.S. Congress of the FDA’s approval process may significantly delay or prevent marketing approval, as well as subject us to more stringent product labeling and post-marketing testing and other requirements. Moreover, the Drug Supply Chain Security Act imposes obligations on manufacturers of pharmaceutical products, among others, related to product tracking and tracing.
Legislation and regulations that, among other things, reduce drug prices or require the implementation of costly compliance measures could result in decreased net revenues from our pharmaceutical products and decrease potential returns from our development efforts, and we cannot predict what legislation will be enacted in the future. Further, it is possible that additional governmental action is taken in response to the COVID-19 pandemic.
Governments outside the United States tend to impose strict price controls, which may adversely affect our revenues, if any.
In international markets, reimbursement and health care payment systems vary significantly by country, and many countries have instituted price ceilings on specific products and therapies. In some countries, particularly the countries of the EU, the pricing of prescription pharmaceuticals is subject to governmental control. In these countries, pricing negotiations with governmental authorities can take considerable time after the receipt of marketing approval for a product. To obtain coverage and reimbursement or pricing approval in some countries, we may be required to conduct a
62
clinical trial that compares the cost-effectiveness of our product candidate to other available therapies. There can be no assurance that our products will be considered cost-effective by third-party payers, that an adequate level of reimbursement will be available or that the third-party payers’ reimbursement policies will not adversely affect our ability to sell our products profitably. If reimbursement of our products is unavailable or limited in scope or amount, or if pricing is set at unsatisfactory levels, our business could be harmed, possibly materially.
Our employees, independent contractors, consultants, and commercial partners may engage in misconduct or other improper activities, including noncompliance with regulatory standards and requirements, which could have a material adverse effect on our business.
We are exposed to the risk of fraud or other misconduct by our employees, independent contractors, consultants and commercial partners. Misconduct by such individuals could include intentional failures to:
| ● | comply with FDA regulations and other similar foreign regulations; |
| ● | provide true, complete and accurate information to the FDA; |
| ● | comply with manufacturing standards; |
| ● | comply with federal and state data privacy, security, fraud and abuse and other healthcare laws and regulations in the United States and similar foreign laws; |
| ● | report financial information or data accurately; or |
| ● | disclose unauthorized activities to us. |
In particular, the promotion, sales and marketing of healthcare items and services, as well as certain business arrangements in the healthcare industry, are subject to extensive laws and regulations intended to prevent fraud, misconduct, kickbacks, self-dealing and other abusive practices. These laws and regulations may restrict or prohibit a wide range of pricing, discounting, marketing and promotion, including off label uses of our products, structuring and commission(s), certain customer incentive programs, patient assistance programs, and other business arrangements generally. Third party misconduct could also involve the improper use or misrepresentation of information obtained in the course of clinical trials, which could result in regulatory sanctions and serious harm to our reputation. It is not always possible to identify and deter such misconduct, and the precautions we take to detect and prevent this activity may not be effective in controlling unknown or unmanaged risks or losses or in protecting us from governmental investigations or other actions or lawsuits stemming from a failure to be in compliance with such laws or regulations. If any such actions are instituted against us, and we are not successful in defending ourselves or asserting our rights, those actions could have a significant impact on our business and financial results, including the imposition of civil, criminal and administrative penalties, damages, disgorgement, monetary fines, possible exclusion from participation in Medicare, Medicaid and other federal healthcare programs, individual imprisonment, contractual damages, reputational harm, diminished profits and future earnings, additional reporting requirements and/or oversight if we become subject to a corporate integrity agreement or similar agreement to resolve allegations of non-compliance with these laws, and curtailment or restructuring of our operations, any of which could adversely affect our ability to operate our business and our results of operations.
Our business involves the use of hazardous materials and we must comply with environmental laws and regulations, which can be expensive and restrict how we do business.
Our manufacturing activities involve the controlled storage, use and disposal of hazardous materials, including the components of our products, product candidates and other hazardous compounds. We are subject to federal, state and local laws and regulations governing the use, manufacture, storage, handling, release and disposal of, and exposure to, these hazardous materials. Violation of these laws and regulations could lead to substantial fines and penalties. Although we believe that our safety procedures for handling and disposing of these materials comply with the standards prescribed
63
by these laws and regulations, we cannot eliminate the risk of accidental contamination or injury from these materials. In the event of an accident, state or federal authorities may curtail our use of these materials and interrupt our business operations. In addition, we could become subject to potentially material liabilities relating to the investigation and cleanup of any contamination, whether currently unknown or caused by future releases.
Although we maintain workers’ compensation insurance to cover us for costs and expenses we may incur due to injuries to our employees resulting from the use of hazardous materials, this insurance may not provide adequate coverage against potential liabilities. We do not maintain insurance for environmental liability or toxic tort claims that may be asserted against us in connection with our storage or disposal of biological, hazardous or radioactive materials.
In addition, we may incur substantial costs in order to comply with current or future environmental, health and safety laws and regulations. These current or future laws and regulations may impair our research, development or production efforts. Our failure to comply with these laws and regulations also may result in substantial fines, penalties or other sanctions.
Risks Related to Intellectual Property
It is difficult and costly to protect our proprietary rights and as a result we may not be able to ensure their protection and all patents will eventually expire.
Our commercial success will depend in part on obtaining and maintaining patent protection and trade secret protection for difelikefalin for our KORSUVA injection or other product candidates and for any other product candidates that we may develop, license or acquire and the methods we use to manufacture them, as well as successfully defending these patents and trade secrets against third-party challenges. We will only be able to protect our technologies from unauthorized use by third parties to the extent that valid and enforceable patents or trade secrets cover them.
The patent prosecution process is expensive and time-consuming, and we may not be able to file and prosecute to issuance all necessary or desirable patent applications at a reasonable cost or in a timely manner. It is also possible that we will fail to identify patentable aspects of our R&D output before it is too late to obtain patent protection. Moreover, should we enter into additional collaborations we may be required to consult with or cede control to collaborators regarding the prosecution, maintenance and enforcement of our patents. Therefore, these patents and applications may not be successfully prosecuted to issuance and enforced in a manner consistent with the best interests of our business. The patent positions of pharmaceutical and biotechnology companies can be highly uncertain and involve complex legal and factual questions for which important legal principles remain unresolved. No consistent policy regarding the breadth of claims allowed in pharmaceutical or biotechnology patents has emerged to date in the United States. The patent situation outside the United States is even more uncertain. Changes in either the patent laws or in interpretations of patent laws in the United States and other countries may diminish the value of our intellectual property. Accordingly, we cannot predict the breadth of claims that may be allowed or enforced in our patents or in third-party patents. The degree of future protection for our proprietary rights is uncertain, because legal means afford only limited protection and may not adequately protect our rights or permit us to gain or keep our competitive advantage. Moreover, the patent application process is also subject to numerous risks and uncertainties, and there can be no assurance that we or any of our future development partners will be successful in protecting difelikefalin and any other product candidates that we may develop, license or acquire by obtaining and defending patents. For example:
| ● | we may not have been the first to make the inventions covered by each of our pending patent applications and issued patents; |
| ● | we may not have been the first to file patent applications for these inventions; |
| ● | others may independently develop similar or alternative technologies or duplicate any of our product candidates or technologies; |
| ● | it is possible that none of the pending patent applications will result in issued patents; |
64
| ● | the issued patents covering our product candidates may not provide a basis for commercially viable active products, may not provide us with any competitive advantages, or may be challenged by third parties; |
| ● | we may not develop additional proprietary technologies that are patentable; |
| ● | patents of others may have an adverse effect on our business; |
| ● | competitors may file trademark infringement claims or challenges to the validity of our trademark(s); |
| ● | noncompliance with governmental patent agencies requirements can result in abandonment or lapse of a patent or patent application, resulting in partial or complete loss of patent rights in the relevant jurisdiction, potentially allowing competitors to enter the market earlier than would otherwise have been the case; |
| ● | our competitors, many of whom have substantially greater resources than we do and many of whom have made significant investments in competing technologies, may seek or may have already obtained patents that will limit, interfere with, or eliminate our ability to make, use, and sell our potential product candidates; or |
| ● | there may be significant pressure on the U.S. government and international governmental bodies to limit the scope of available patent protection both inside and outside the United States for disease treatments that prove successful, as a matter of public policy regarding worldwide health concerns. |
Recent patent reform legislation could increase the uncertainties and costs surrounding the prosecution of our patent applications and the enforcement or defense of our issued patents. On September 16, 2011, the Leahy-Smith America Invents Act, or the Leahy-Smith Act, was signed into law. The Leahy-Smith Act includes a number of significant changes to United States patent law. These include provisions that affect the way patent applications are prosecuted and may also affect patent litigation. The United States Patent Office has developed new regulations and procedures to govern administration of the Leahy-Smith Act, and many of the substantive changes to patent law associated with the Leahy-Smith Act, including and in particular, the first to file provisions, became effective on March 16, 2013. The Leahy-Smith Act and its implementation could increase the uncertainties and costs surrounding the prosecution of our currently pending and future patent applications and the enforcement or defense of our issued patents, all of which could have a material adverse effect on our business and financial condition.
Patent applications in the United States are generally maintained in confidence for at least 18 months after their earliest effective filing date and in certain circumstances not until granted when no foreign counterpart patent applications are filed. Furthermore, published patent applications may issue at a later date with new and/or amended claims substantially different from those published earlier. Consequently, we cannot be certain we were the first to invent or the first to file patent applications on difelikefalin or any other product candidates that we may develop, license or acquire.
Until recent changes to the U.S. Patent Laws, patents and patent applications relating to substantially similar claimed inventions were potentially subject to interference proceedings to determine the first applicant to invent the claimed subject matter. For an interference to be declared against our patents and patent applications, any such interference would be under the 1952 law which was eliminated by the America Invents Act, or AIA, enacted in 2011 and fully effective in 2013. Such an interference would therefore have to relate to a patent or application with an effective filing date before March 16, 2013. No interference with such a patent or application has been declared to date. Therefore, it seems extremely unlikely that we may have to participate in interference proceedings declared by the USPTO to determine priority of invention in the United States against one or more parties claiming the same or similar invention. However, in the unlikely event that such interference was to be declared, the costs of these proceedings could be substantial and it is possible that our efforts would be unsuccessful, resulting in a material adverse effect on our U.S. patent position. The results of these types of proceedings could reduce the scope of, or invalidate, our patent rights, allow third parties to commercialize our technology or products and compete directly with us, without payment to us, or result in our inability to manufacture or commercialize products without infringing third-party patent rights. In addition, if the breadth or strength of protection provided by our patents and patent applications is threatened, it could dissuade
65
companies from collaborating with us to license, develop or commercialize current or future product candidates. Such results could have a material adverse effect on our results of operations.
In addition, the patentability of claims in pending patent applications covering KORSUVA injection or other difelikefalin-based product can be challenged by third parties during prosecution in the USPTO under the new AIA law of 2013, for example by third party observations and derivation proceedings, and the validity of claims in issued patents can be challenged by third parties in various post-grant proceedings such as Post-Grant Review, Inter-partes Reexamination, and Inter-partes Review proceedings.
Furthermore, we may not have identified all United States and foreign patents or published applications that affect our business either by blocking our ability to commercialize our drugs or by covering similar technologies that affect our drug market. In addition, some countries, including many in Europe, do not grant patent claims directed to methods of treating humans, and in these countries patent protection may not be available at all to protect our product candidates. Even if patents issue, we cannot guarantee that the claims of those patents will be valid and enforceable or provide us with any significant protection against competitive products, or otherwise be commercially valuable to us.
We also rely on trade secrets to protect our technology, particularly where we do not believe patent protection is appropriate or obtainable. However, trade secrets are difficult to protect. While we use reasonable efforts to protect our trade secrets, our licensors, employees, consultants, contractors, outside scientific collaborators and other advisors may unintentionally or willfully disclose our information to competitors. Enforcing a claim that a third party illegally obtained and is using our trade secrets is expensive and time consuming, and the outcome is unpredictable. In addition, courts outside the United States are sometimes less willing to protect trade secrets. Moreover, our competitors may independently develop equivalent knowledge, methods and know-how.
If we fail to obtain or maintain patent protection or trade secret protection for difelikefalin or any other product candidate that we may develop, license or acquire, third parties could use our proprietary information, which could impair our ability to compete in the market and adversely affect our ability to generate revenues and achieve profitability.
Even if our patent applications issue as patents, they may not issue in a form that will provide us with any meaningful protection, prevent competitors from competing with us or otherwise provide us with any competitive advantage. Our competitors may be able to circumvent our owned or licensed patents by developing similar or alternative technologies or products in a non-infringing manner.
The issuance of a patent is not conclusive as to its inventorship, scope, validity or enforceability, and our owned and licensed patents may be challenged in the courts or patent offices in the United States and abroad. Such challenges may result in loss of exclusivity or freedom to operate or in patent claims being narrowed, invalidated or held unenforceable, in whole or in part, which could limit our ability to stop others from using or commercializing similar or identical technology and products, or limit the duration of the patent protection of our technology and products. Given the amount of time required for the development, testing and regulatory review of new product candidates, patents protecting such product candidates might expire before or shortly after such product candidates are commercialized. As a result, our owned and licensed patent portfolio may not provide us with sufficient rights to exclude others from commercializing products similar or identical to ours.
If we or any current or future collaboration partner are sued for infringing intellectual property rights of third parties, it will be costly and time consuming, and an unfavorable outcome in any litigation would harm our business.
Our ability to develop, manufacture, market and sell KORSUVA injection or any of our other current of future product candidates depends upon our ability to avoid infringing the proprietary rights of third parties, and our commercial success depends upon our ability, and the ability of our collaborators, to develop, manufacture, market and sell our product candidates and use our proprietary technologies without infringing the proprietary rights of third parties. There is considerable intellectual property litigation in the biotechnology and pharmaceutical industries. Numerous U.S. and foreign issued patents and pending patent applications, which are owned by third parties, exist in the general field of pain management and cover the use of numerous compounds and formulations in our targeted markets. Third parties
66
may assert infringement claims against us based on existing patents or patents that may be granted in the future. Because of the uncertainty inherent in any patent or other litigation involving proprietary rights, we and our licensors may not be successful in defending intellectual property claims by third parties, which could have a material adverse effect on our results of operations. Regardless of the outcome of any litigation, defending the litigation may be expensive, time-consuming and distracting to management. In addition, because patent applications can take many years to issue, there may be currently pending applications, unknown to us, which may later result in issued patents that KORSUVA injection or our other current or future product candidates may infringe. There could also be existing patents of which we are not aware that KORSUVA injection or our other current or future product candidates may inadvertently infringe.
There is a substantial amount of litigation involving patent and other intellectual property rights in the biotechnology and biopharmaceutical industries generally. If a third-party claims that we infringe on their products or technology, we could face a number of issues, including:
| ● | infringement and other intellectual property claims which, with or without merit, can be expensive and time consuming to litigate and can divert management’s attention from our core business; |
| ● | substantial damages for past infringement which we may have to pay if a court decides that our product infringes on a competitor’s patent; |
| ● | a court prohibiting us from selling or licensing our product unless the patent holder licenses the patent to us, which it would not be required to do; |
| ● | if a license is available from a patent holder, we may have to pay substantial royalties or grant cross licenses to our patents; and |
| ● | redesigning our processes so they do not infringe, which may not be possible or could require substantial funds and time. |
If we are found to infringe a third party’s intellectual property rights, we could be required to obtain a license from such third party to continue developing and marketing our products and technology. However, we may not be able to obtain any required license on commercially reasonable terms or at all. Even if we were able to obtain a license, it could be non-exclusive, thereby giving our competitors access to the same technologies licensed to us. We could be forced, including by court order, to cease commercializing the infringing technology or product. In addition, we could be found liable for monetary damages, including treble damages and attorneys’ fees if we are found to have willfully infringed a patent. A finding of infringement could prevent us from commercializing our product candidates or force us to cease some of our business operations, which could materially harm our business. Claims that we have misappropriated the confidential information or trade secrets of third parties could have a similar negative impact on our business.
We may be involved in lawsuits to protect or enforce our patents or the patents of our licensors, which could be expensive, time consuming and may ultimately be unsuccessful.
Competitors may infringe our issued patents or other intellectual property. To counter infringement or unauthorized use, we may be required to file infringement claims, which can be expensive and time consuming. Any claims we assert against perceived infringers could provoke these parties to assert counterclaims against us alleging that we infringe their patents. In addition, in a patent infringement proceeding, a court may decide that a patent of ours is invalid or unenforceable, in whole or in part, construe the patent’s claims narrowly or refuse to stop the other party from using the technology at issue on the grounds that our patents do not cover the technology in question. An adverse result in any litigation proceeding could put one or more of our patents at risk of being invalidated or interpreted narrowly. Furthermore, because of the substantial amount of discovery required in connection with intellectual property litigation, there is a risk that some of our confidential information could be compromised by disclosure during this type of litigation.
67
Most of our competitors are larger than we are and have substantially greater resources. They are, therefore, likely to be able to sustain the costs of complex patent litigation longer than we could. In addition, the uncertainties associated with litigation could have a material adverse effect on our ability to raise the funds necessary to continue our clinical trials, continue our internal research programs, in-license needed technology, or enter into development partnerships that would help us bring our product candidates to market.
We may need to license certain intellectual property from third parties, and such licenses may not be available or may not be available on commercially reasonable terms.
A third party may hold intellectual property, including patent rights that are important or necessary to the development or commercialization of our products. It may be necessary for us to use the patented or proprietary technology of third parties to commercialize our products, in which case we would be required to obtain a license from these third parties. Such a license may not be available on commercially reasonable terms or at all, which could materially harm our business.
We may be subject to claims that our employees have wrongfully used or disclosed alleged trade secrets of their former employers.
As is common in the biotechnology and pharmaceutical industry, we employ individuals who were previously employed at other biotechnology or pharmaceutical companies, including our competitors or potential competitors. Although no claims against us are currently pending, we may be subject to claims that these employees or we have inadvertently or otherwise used or disclosed trade secrets or other proprietary information of their former employers. Litigation may be necessary to defend against these claims. Even if we are successful in defending against these claims, litigation could result in substantial costs and be a distraction to management.
We may not be able to protect our intellectual property rights throughout the world.
Filing, prosecuting and defending patents on product candidates in all countries throughout the world would be prohibitively expensive, and our intellectual property rights in some countries outside the United States can be less extensive than those in the United States. In addition, the laws of some foreign countries do not protect intellectual property rights to the same extent as federal and state laws in the United States. Consequently, we may not be able to prevent third parties from practicing our inventions in all countries outside the United States, or from selling or importing products made using our inventions in and into the United States or other jurisdictions. Competitors may use our technologies in jurisdictions where we have not obtained patent protection to develop their own products and further, may export otherwise infringing products to territories where we have patent protection, but enforcement rights are not as strong as those in the United States. These products may compete with our product candidates and our patents or other intellectual property rights may not be effective or sufficient to prevent them from competing.
Many companies have encountered significant problems in protecting and defending intellectual property rights in foreign jurisdictions. The legal systems of certain countries do not favor the enforcement of patents and other intellectual property protection, which could make it difficult for us to stop the infringement of our patents generally. Proceedings to enforce our patent rights in foreign jurisdictions could result in substantial costs and divert our efforts and attention from other aspects of our business, could put our patents at risk of being invalidated or interpreted narrowly and our patent applications at risk of not issuing and could provoke third parties to assert claims against us. We may not prevail in any lawsuits that we initiate and the damages or other remedies awarded, if any, may not be commercially meaningful. Accordingly, our efforts to enforce our intellectual property rights around the world may be inadequate to obtain a significant commercial advantage from the intellectual property that we develop or license.
The validity and enforceability of the patents and applications that cover KORSUVA injection and our difelikefalin product candidates can be challenged by competitors.
For KORSUVA injection and in the event that an Oral KORSUVA (difelikefalin) or any future product candidate is approved by the FDA, one or more third parties may challenge the patents covering these products and product candidates, which could result in the invalidation of, or render unenforceable, some or all of the relevant patent claims.
68
For example, if a third party files an Abbreviated New Drug Application, or ANDA, for a generic drug product containing difelikefalin, and relies in whole or in part on studies conducted by or for us, the third party will be required to certify to the FDA that either: (1) the patents listed in the Orange Book have expired; (2) the listed patents have not expired, but will expire on a particular date and approval is sought after patent expiration; or (3) the listed patents are invalid or will not be infringed by the manufacture, use or sale of the third-party’s generic drug product. A certification that the new product will not infringe the Orange Book-listed patents for difelikefalin, or that such patents are invalid, is called a paragraph IV certification. If the third party submits a paragraph IV certification to the FDA, a notice of the paragraph IV certification must also be sent to us once the third-party’s ANDA is accepted for filing by the FDA. We may then initiate a lawsuit to defend the patents identified in the notice. The filing of a patent infringement lawsuit within 45 days of receipt of the notice automatically prevents the FDA from approving the third-party’s ANDA until the earliest of 30 months or the date on which the patent expires, the lawsuit is settled, or the court reaches a decision in the infringement lawsuit in favor of the third party. If we do not file a patent infringement lawsuit within the required 45-day period, the third-party’s ANDA will not be subject to the 30-month stay. Litigation or other proceedings to enforce or defend intellectual property rights are often very complex in nature, may be very expensive and time-consuming, may divert our management’s attention from our core business, and may result in unfavorable results that could adversely impact our ability to prevent third parties from competing with our products.
Risks Related to Employee Matters and Managing Growth
Our internal information technology systems, or those of our CROs, contract manufacturers or other contractors or consultants, may fail or suffer cybersecurity breaches, loss or leakage of data and other disruptions, which could result in a material disruption of our development programs, commercialization efforts, compromise sensitive information related to our business or prevent us from accessing critical information, potentially exposing us to liability, which could adversely affect our business.
We are increasingly dependent upon information technology systems, infrastructure and data to operate our business. In the ordinary course of business, we collect, store and transmit confidential information (including but not limited to intellectual property, proprietary business information and personal information). It is critical that we do so in a secure manner to maintain the confidentiality and integrity of such confidential information. We also have outsourced elements of our operations to third parties, and as a result we manage a number of third-party contractors who have access to our confidential information.
Despite the implementation of cybersecurity measures, given their size and complexity and the increasing amounts of confidential information that they maintain, our internal information technology systems and those of our third-party CROs, contract manufacturers and other contractors and consultants are potentially vulnerable to breakdown or other damage or interruption from service interruptions, system malfunction, natural disasters, terrorism, war and telecommunication and electrical failures, as well as cybersecurity breaches from inadvertent or intentional actions by our employees, contractors, consultants, business partners and/or other third parties, or from cyber-attacks by malicious third parties (including the deployment of harmful malware, ransomware, denial-of-service attacks, social engineering and other means to affect service reliability and threaten the confidentiality, integrity and availability of information), which may compromise our system infrastructure or lead to data leakage. Cybersecurity risks have significantly increased in recent years in part because of the proliferation of new technologies, the use of the internet and telecommunication technologies to conduct financial transactions, especially as more employees are working remotely, and the increased sophistication and activities of organized crime, hackers, terrorists, nation-states and other external parties. To the extent that any disruption or cybersecurity breach were to result in a loss of, or damage to, our data or applications, or inappropriate disclosure of confidential or proprietary information, we could incur liability and reputational damage and the further development and commercialization of our product candidates could be delayed.
While we have not experienced any such system failure, accident or cybersecurity breach to date, we cannot assure you that our data protection efforts and our investment in information technology will prevent significant breakdowns, data leakages, breaches in our systems or other cyber incidents that could adversely affect our business. For example, if such an event were to occur and cause interruptions in our operations, it could result in a material disruption of our programs and the development and commercialization of KORSUVA injection, if approved, could be delayed. In addition, the loss of clinical trial data could result in delays in our marketing approval efforts and significantly increase
69
our costs to recover or reproduce the data. Furthermore, significant disruptions of our internal information technology systems or cybersecurity breaches could result in the loss, misappropriation and/or unauthorized access, use, or disclosure of, or the prevention of access to, confidential information (including trade secrets or other intellectual property, proprietary business information and personal information), which could result in financial, legal, business and reputational harm to us. For example, any such event that leads to unauthorized access, use, or disclosure of personal information, including personal information regarding our clinical trial subjects or employees, could harm our reputation directly, compel us to comply with federal and/or state breach notification laws and foreign law equivalents, subject us to mandatory corrective action, and otherwise subject us to liability under laws and regulations that protect the privacy and security of personal information, which could result in significant legal and financial exposure and reputational damages that could adversely affect our business.
We may need to significantly increase the size of our organization, and we may experience difficulties in managing growth.
As of February 24, 2022, we had 84 employees. Our management and personnel systems and facilities currently in place may not be adequate to support future growth. In addition, we may not be able to recruit and retain qualified personnel in the future, particularly for sales and marketing positions, due to competition for personnel among pharmaceutical businesses, and the failure to do so could have a significant negative impact on our future product revenues and business results. Our need to effectively manage our operations, growth and various projects requires that we:
| ● | ensure that our consultants and other service providers successfully carry out their contractual obligations, provide high quality results, and meet expected deadlines; |
| ● | continue to carry out our own contractual obligations to our licensors and other third parties; and |
| ● | continue to improve our operational, financial and management controls, reporting systems and procedures. |
We may be unable to successfully implement these tasks on a larger scale and, accordingly, may not achieve our development and commercialization goals.
We depend on skilled personnel to operate our business effectively in a rapidly changing market, and if we are unable to retain existing or hire additional personnel when needed, or manage transitions among members of our leadership team, our ability to develop and sell our products could be harmed.
We may not be able to attract or retain qualified management and commercial, scientific and clinical personnel due to the intense competition for qualified personnel among biotechnology, pharmaceutical and other businesses. If we are not able to attract and retain necessary personnel to accomplish our business objectives, we may experience constraints that will significantly impede the achievement of our development objectives, our ability to raise additional capital and our ability to implement our business strategy.
Our industry has experienced a high rate of turnover of management personnel in recent years. We are highly dependent on the skills and leadership of our management team, including our President and CEO. Most recently, we appointed a new President and CEO in November 2021, at which time our former President and CEO, who had served in such position since 2004, transitioned to the role of Senior Advisor to the Company. This transition may be disruptive to our business. Further, our senior management may terminate their employment with us at any time. If we are unable to execute an orderly transition and successfully integrate our new CEO into our management team, or if we lose one or more members of our senior management team, our ability to successfully implement our business strategy could be seriously harmed. Replacing these employees may be difficult and may take an extended period of time because of the limited number of individuals in our industry with the breadth of skills and experience required to develop, gain regulatory approval of and commercialize products successfully. Competition to hire from this limited pool is intense, and we may be unable to hire, train, retain or motivate additional key personnel. We do not maintain “key person” insurance for any of our executives or other employees.
70
If we fail to maintain proper and effective internal controls, our ability to produce accurate financial statements on a timely basis could be impaired.
We are subject to the reporting requirements of the Securities Exchange Act of 1934, as amended, the Sarbanes-Oxley Act of 2002 and the rules and regulations of The Nasdaq Global Market. Pursuant to Section 404 of the Sarbanes-Oxley Act of 2002, or Section 404, we are now required to perform system and process evaluation and testing of our internal control over financial reporting to allow our management to report on the effectiveness of our internal control over financial reporting and we are also required to have our independent registered public accounting firm issue an opinion on the effectiveness of our internal control over financial reporting on an annual basis.
During the evaluation and testing process, if we identify one or more material weaknesses in our internal control over financial reporting, we will be unable to assert that our internal control over financial reporting is effective. Further, we may in the future discover weaknesses in our system of internal financial and accounting controls and procedures that could result in a material misstatement of our financial statements. Moreover, our internal controls over financial reporting will not prevent or detect all errors and all fraud. A control system, no matter how well designed and operated, can provide only reasonable, not absolute, assurance that the control system’s objectives will be met. Because of the inherent limitations in all control systems, no evaluation of controls can provide absolute assurance that misstatements due to error or fraud will not occur or that all control issues and instances of fraud will be detected. Moreover, we are aware that the remote working arrangements implemented in connection with the COVID-19 pandemic potentially present new areas of risk, including cyber, privacy and productivity risks, and we are carefully monitoring any impact to our internal controls and procedures.
If we are unable to assert that our internal control over financial reporting is effective, or if our independent registered public accounting firm is unable to express an opinion on the effectiveness of our internal control over financial reporting, investors could lose confidence in the reliability of our financial statements, the market price of our stock could decline and we could be subject to sanctions or investigations by The Nasdaq Global Market, the SEC or other regulatory authorities.
Risks Related to Ownership of Our Common Stock
The market price of our common stock has been, and is likely to continue to be, highly volatile, and you may not be able to resell your shares at or above the price you paid for them.
Since our initial public offering in January 2014, our stock price has been volatile and it is likely that the trading price of our common stock will continue to be volatile. As a result of this volatility, investors may not be able to sell their common stock at or above the price paid for the shares. The market price for our common stock may be influenced by many factors, including:
| ● | delays in the commencement, enrollment and ultimate completion of our clinical trials, including our planned trials for Oral KORSUVA (difelikefalin); |
| ● | any delay or refusal on the part of the FDA in approving an NDA for our other current or future product candidates; |
| ● | the commercial success of KORSUVA injection and, if approved by the FDA, Oral KORSUVA (difelikefalin) or any future product candidates; |
| ● | results of clinical trials of Oral KORSUVA (difelikefalin), such as our announcement of topline results from the Phase 2 clinical trial of Oral KORSUVA (difelikefalin) tablets for the treatment of moderate-to-severe pruritus in mild-to-severe AD in April 2021, or any future product candidate or those of our competitors; |
| ● | actual or anticipated variations in quarterly or annual operating results; |
71
| ● | failure to meet or exceed financial projections we provide to the public; |
| ● | failure to meet or exceed the estimates and projections of the investment community, including securities analysts; |
| ● | introduction of competitive products or technologies; |
| ● | changes or developments in laws or regulations applicable to our product candidates; |
| ● | the perception of the pharmaceutical industry by the public, legislatures, regulators and the investment community; |
| ● | general trends in our industry or economic and market conditions and overall fluctuations in U.S. equity markets, including as a result of the ongoing COVID-19 pandemic; |
| ● | developments concerning our sources of manufacturing supply, warehousing and inventory control; |
| ● | disputes or other developments relating to patents or other proprietary rights; |
| ● | additions or departures of key scientific or management personnel; |
| ● | announcements of investigations or regulatory scrutiny of our operations or lawsuits filed against us; |
| ● | capital commitments; |
| ● | investors’ general perception of our company and our business; |
| ● | announcements and expectations of additional financing efforts, including the issuance of debt, equity or convertible securities; |
| ● | sales of our common stock, including sales by our directors and officers or significant stockholders; |
| ● | changes in the market valuations of companies similar to us; |
| ● | announcements by us or our competitors of significant acquisitions, strategic partnerships, or divestitures; |
| ● | changes in the structure of healthcare payment systems; and |
| ● | the other factors described in this “Risk Factors” section. |
In addition, the stock market in general, and the market for small pharmaceutical and biotechnology companies in particular, have experienced extreme price and volume fluctuations that have often been unrelated or disproportionate to the operating performance of these companies. Broad market and industry factors, such as those related to the ongoing COVID-19 pandemic, may negatively affect the market price of our common stock, regardless of our actual operating performance.
Further, in the past, stockholders have initiated class action lawsuits against pharmaceutical and biotechnology companies following periods of volatility in the market prices of these companies’ stock. Such litigation, if instituted against us, could cause us to incur substantial costs and divert management’s attention and resources from our business.
72
If equity research analysts cease to publish research or reports about us or if they publish unfavorable research or reports about us, our business or our market, our stock price and trading volume could decline.
The trading market for our common stock is likely to be influenced by the research and reports that equity research analysts publish about us and our business. We do not have any control over the analysts or the content and opinions included in their reports. The price of our stock could decline if one or more equity research analysts downgrade our stock or issue other unfavorable commentary or research. If one or more equity research analysts ceases coverage of our company or fails to publish reports on us regularly, demand for our stock could decrease, which in turn could cause our stock price or trading volume to decline.
Our quarterly operating results may fluctuate significantly.
We expect our operating results to be subject to quarterly fluctuations. Our operating results will be affected by numerous factors, including:
| ● | our or our partners’ or our collaborators’ ability to establish the necessary commercial infrastructure to successfully launch KORSUVA injection without substantial delays, including hiring sales and marketing personnel and contracting with third parties for warehousing, distribution, cash collection and related commercial activities; |
| ● | the successful progress of our clinical trials for Oral KORSUVA (difelikefalin) and other potential future product candidates; |
| ● | whether the FDA requires us to complete additional, unanticipated studies, tests or other activities prior to approving our other current or future product candidates, which would likely further delay any such approval; |
| ● | our ability to identify, enter into and maintain third party manufacturing arrangements capable of manufacturing KORSUVA injection or our other current or future product candidates in commercial quantities; |
| ● | our execution of other collaborative, licensing or similar arrangements and the timing of payments we may make or receive under these arrangements; |
| ● | variations in the level of expenses related to our future development programs; |
| ● | any product liability or intellectual property infringement lawsuit in which we may become involved; |
| ● | regulatory developments affecting KORSUVA injection, Oral KORSUVA (difelikefalin), any of our future product candidates, or the product candidates of our competitors; and |
| ● | for KORSUVA injection, and if Oral KORSUVA (difelikefalin) or any of our future product candidates receives regulatory approval, the level of underlying demand for such product and product candidate and wholesaler buying patterns. |
If our quarterly or annual operating results fall below the expectations of investors or securities analysts, the price of our common stock could decline substantially. Furthermore, any quarterly or annual fluctuations in our operating results may, in turn, cause the price of our stock to fluctuate substantially. We believe that quarterly comparisons of our financial results are not necessarily meaningful and should not be relied upon as an indication of our future performance.
Raising additional funds by issuing securities may cause dilution to existing stockholders and raising funds through lending and licensing arrangements may restrict our operations or require us to relinquish proprietary rights.
Until such time, if ever, as we can generate substantial product revenues, we expect to finance our cash needs through a combination of equity offerings, debt financings, grants and license and development agreements in
73
connection with any collaborations. We do not yet have any committed external source of funds. To the extent that we raise additional capital by issuing equity securities, our existing stockholders’ ownership will be diluted, and the terms of these securities may include liquidation or other preferences that adversely affect your rights as a common stockholder. Debt financing and preferred equity financing, if available, may involve agreements that include covenants limiting or restricting our ability to take specific actions, such as incurring additional debt, making capital expenditures or declaring dividends.
If we raise additional funds through collaborations, strategic alliances or marketing, distribution or licensing arrangements with third parties, we may have to relinquish valuable rights to our technologies, future revenue streams, research programs or KORSUVA injection or product candidates or grant licenses on terms that may not be favorable to us. Any debt financing that we enter into may involve covenants that restrict our operations. These restrictive covenants may include limitations on additional borrowing and specific restrictions on the use of our assets as well as prohibitions on our ability to create liens, pay dividends, redeem our stock or make investments. If we are unable to raise additional funds through equity or debt financings when needed, we may be required to delay, limit, reduce or terminate our product development or future commercialization efforts or grant rights to develop and market product candidates that we would otherwise prefer to develop and market ourselves.
The use of our net operating loss carryforwards and research tax credits may be limited.
A portion of our net operating loss, or NOL, carryforwards and R&D tax credits may expire and not be used. As of December 31, 2021, we had federal and state NOL carryforwards of approximately $443.1 million and $347.3 million, respectively, and we also had federal and state R&D tax credit carryforwards of approximately $19.9 million and $5.5 million, respectively. Our NOL carryforwards will begin expiring in 2026 for federal purposes (to the extent such federal NOLs are generated in taxable years beginning on or before December 31, 2017) and 2027 for state purposes if we have not used them prior to that time, and our federal R&D tax credits will begin expiring in 2025 unless previously used. The federal NOLs arising in 2018 and forward have an unlimited carryforward period and losses from 2018-2020 may be carried back five years due to the Coronavirus Aid, Relief, and Economic Security Act of 2020, or the CARES Act. It is uncertain if and to what extent various states will conform to the TCJA, as modified by the CARES Act. To the extent that we have not exchanged our Connecticut R&D tax credits for a tax refund, those tax credits carry forward indefinitely. Additionally, our ability to use any NOL and R&D tax credit carryforwards to offset taxable income or tax, respectively, in the future will be limited under Internal Revenue Code Sections 382 and 383, respectively, if we have a cumulative change in ownership of our stock of more than 50% within a three-year period. The completion of our initial public offering in 2014 and our follow-on public offerings in 2015, 2017, 2018 and 2019, together with private placements and other transactions that have occurred, may have triggered such ownership changes. We conducted a 382 analysis in the first quarter of 2021. This analysis showed a limited change of ownership had occurred, and the amount of NOL carryforwards and R&D tax credits that could be utilized annually in the future to offset taxable income or tax, respectively. In addition, since we will need to raise substantial additional funding to finance our operations, we may undergo ownership changes in the future. Any such annual limitation may significantly reduce the utilization of the NOL carryforwards and R&D tax credits before they expire. In addition, certain states have in the past suspended use of NOL carryforwards for certain taxable years (including Connecticut which currently limits the use of NOL carryforwards by 50% and without limitation legislation enacted by California in June 2020 that suspends the use of California NOLs and limits the use of California R&D tax credits for certain years), and other states are considering similar measures. As a result, we may incur higher state income tax expense in the future. Depending on our future tax position, limitations on our ability to use NOL carryforwards in states in which we are subject to income tax could have an adverse impact on our results of operations and financial condition.
New or future changes to tax laws could materially adversely affect our company.
On December 22, 2017, President Trump signed into law the TCJA, which significantly amends the Internal Revenue Code of 1986, which was modified by the CARES Act. We continue to examine the impact these changes may have on our business. Notwithstanding the reduction in the corporate income tax rate, the overall impact of the TCJA and CARES Act, or any other future changes in tax laws, is uncertain and our business and financial condition could be adversely affected. For example, proposals have recently been made in Congress (which have not yet been enacted) that
74
include tax law changes that could have a material adverse impact on us. The impact of the TCJA and CARES Act and any future changes in tax laws on holders of our common stock is also uncertain and could be adverse.
Because we do not intend to pay dividends on our common stock, your returns will be limited to any increase in the value of our stock.
We have never declared or paid any cash dividends on our capital stock. We currently intend to retain all available funds and any future earnings to support our operations and finance the growth and development of our business and do not anticipate declaring or paying any cash dividends on our common stock for the foreseeable future. Any return to stockholders will therefore be limited to the appreciation of their stock, if any. Investors seeking cash dividends should not purchase our common stock.
Provisions in our corporate charter documents and under Delaware law may prevent or frustrate attempts by our stockholders to change our management and hinder efforts to acquire a controlling interest in us, and the market price of our common stock may be lower as a result.
There are provisions in our certificate of incorporation and bylaws, as amended, that may make it difficult for a third party to acquire, or attempt to acquire, control of our company, even if a change in control was considered favorable by you and other stockholders. For example, our Board of Directors has the authority to issue up to 5,000,000 shares of preferred stock and to fix the price, rights, preferences, privileges, and restrictions of the preferred stock without any further vote or action by our stockholders. The issuance of shares of preferred stock may delay or prevent a change in control transaction. As a result, the market price of our common stock and the voting and other rights of our stockholders may be adversely affected. An issuance of shares of preferred stock may result in the loss of voting control to other stockholders.
Our charter documents also contain other provisions that could have an anti-takeover effect, including:
| ● | our Board of Directors are divided into three classes, with only one class of directors elected each year; |
| ● | our stockholders are entitled to remove directors only for cause upon a 66 2/3% vote; |
| ● | our stockholders are not permitted to take actions by written consent; |
| ● | our stockholders are not permitted to call a special meeting of stockholders; and |
| ● | our stockholders must give us advance notice of their intent to nominate directors or submit proposals for consideration at stockholder meetings. |
In addition, we are subject to the anti-takeover provisions of Section 203 of the Delaware General Corporation Law, which regulates corporate acquisitions by prohibiting Delaware corporations from engaging in specified business combinations with particular stockholders of those companies. These provisions could discourage potential acquisition proposals and could delay or prevent a change in control transaction. They could also have the effect of discouraging others from making tender offers for our common stock, including transactions that may be in your best interests. These provisions may also prevent changes in our management or limit the price that investors are willing to pay for our stock.
Item 1B. Unresolved Staff Comments.
None.
Item 2. Properties.
Our principal offices occupy approximately 36,000 square feet of office space in Stamford, Connecticut under leases that expire in December 2023. We believe that the office space in Stamford is suitable and adequate to meet our
75
current needs and to allow for expansion as we increase our headcount. See Note 18 of Notes to Financial Statements, Commitments and Contingencies, in this Annual Report on Form 10-K.
Item 3. Legal Proceedings.
From time to time, we may become subject to arbitration, litigation or claims arising in the ordinary course of business. We are not currently a party to any arbitration or legal proceeding that, if determined adversely to us, would have a material adverse effect on our business, operating results or financial condition. The results of any future claims or proceedings cannot be predicted with certainty, and regardless of the outcome, litigation can have an adverse impact on us because of defense and litigation costs, diversion of management resources, and other factors.
Item 4. Mine Safety Disclosures.
Not applicable.
PART II
Item 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities.
Market Information for Common Stock
Our common stock is traded on The Nasdaq Global Market under the ticker symbol “CARA”.
Stockholders
As of February 24, 2022, there were 31 holders of record of our common stock. This number does not reflect the beneficial holders of our common stock who hold shares in street name through brokerage accounts or other nominees.
Dividend Policy
We have never declared or paid any cash dividends on our capital stock. We currently intend to retain all available funds and any future earnings to support our operations and finance the growth and development of our business. We do not intend to pay cash dividends on our common stock for the foreseeable future. Any future determination related to dividend policy will be made at the discretion of our Board of Directors and will depend on, among other factors, our results of operations, financial condition, capital requirements, contractual restrictions, business prospects and other factors our Board of Directors may deem relevant.
Stock Performance
The following graph compares cumulative total return of our common stock with the cumulative total return of (i) the Nasdaq Composite Index, and (ii) the Nasdaq Biotechnology Index. The graph assumes (a) $100 was invested on December 31, 2016 in each of our common stock, the stocks comprising the Nasdaq Composite Index and the stocks comprising the Nasdaq Biotechnology Index, and (b) the reinvestment of dividends. The comparisons shown in the
76
graph are based on historical data and the stock price performance shown in the graph is not necessarily indicative of, or intended to forecast, future performance of our stock.
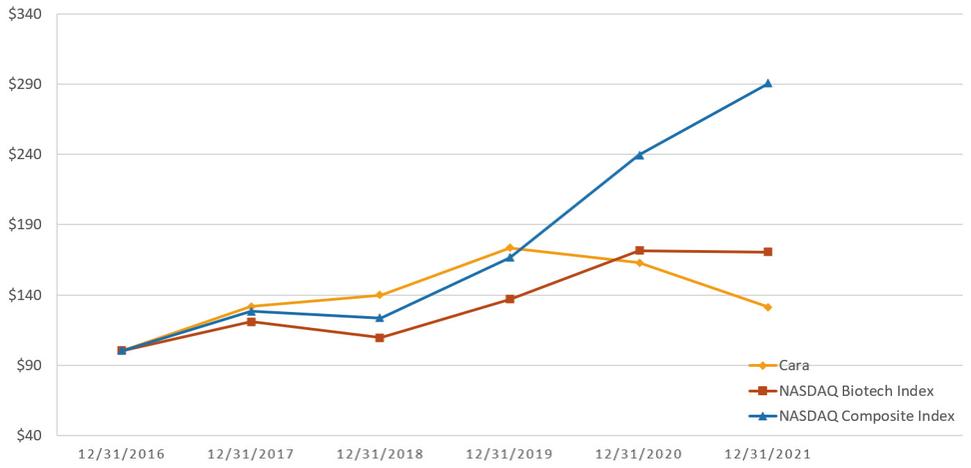
Cumulative Total Return
| 12/31/2016 |
| 12/31/2017 |
| 12/31/2018 |
| 12/31/2019 |
| 12/31/2020 |
| 12/31/2021 | |
Cara Therapeutics, Inc. |
| 100.00 |
| 131.75 |
| 139.94 |
| 173.41 |
| 162.86 | 131.11 | |
Nasdaq Biotechnology |
| 100.00 |
| 121.06 |
| 109.77 |
| 136.56 |
| 171.64 | 170.55 | |
Nasdaq Composite |
| 100.00 |
| 128.24 |
| 123.26 |
| 166.68 |
| 239.42 | 290.63 |
This performance graph shall not be deemed "filed" for purposes of Section 18 of the Securities Exchange Act of 1934, as amended, or the Exchange Act, or incorporated by reference into any filing of ours under the Securities Act, except as shall be expressly set forth by specific reference to such filing.
Recent Sales of Unregistered Securities
In October 2021, after the expiration of the requisite waiting period under the HSR Act, we received the $50.0 million milestone payment from Vifor and issued 3,282,391 shares of our common stock to Vifor at a price of $15.23 per share, in connection with U.S. regulatory approval of KORSUVA injection on August 23, 2021 (see Notes 10 and 12 of Notes to Financial Statements, Stockholders’ Equity and Collaboration and Licensing Agreements, respectively, in this Annual Report on Form 10-K).
Purchases of Equity Securities by the Issuer and Affiliated Purchasers
Not applicable.
Use of Proceeds
Not applicable.
Item 6. [Reserved]
77
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations.
You should read the following discussion and analysis of our financial condition and results of operations together with our financial statements and the related notes appearing at the end of this Annual Report on Form 10-K. Some of the information contained in this discussion and analysis or set forth elsewhere in this Annual Report on Form 10-K, including information with respect to our plans and strategy for our business and related financing, includes forward-looking statements that involve risks and uncertainties. You should read “Cautionary Note Regarding Forward-Looking Statements” and Item 1A. Risk Factors of this Annual Report on Form 10-K for a discussion of material factors that could cause actual results to differ materially from the results described in or implied by the forward-looking statements contained in the following discussion and analysis.
Overview
Introduction
We are an early commercial-stage biopharmaceutical company leading a new treatment paradigm to improve the lives of patients suffering from pruritus. Our novel KORSUVA injection is the first and only FDA-approved treatment for moderate-to-severe pruritus associated with CKD in adults undergoing hemodialysis. We are developing an Oral KORSUVA (difelikefalin) formulation and plan to initiate Phase 3 programs in the first quarter of 2022 for the treatment of pruritus in patients with AD and NDD-CKD. Phase 2 trials of Oral KORSUVA (difelikefalin) are ongoing in PBC and NP patients with moderate-to-severe pruritus.
On August 23, 2021, our lead product, KORSUVA injection, was approved by the FDA for the treatment of moderate-to-severe pruritus associated with CKD in adults undergoing hemodialysis in the United States. We expect commercial launch of KORSUVA injection in April 2022 and associated revenues in the second quarter of 2022.
We have partnered with VFMCRP, a joint venture between Vifor Pharma Group and Fresenius Medical Care, and Vifor to commercialize KORSUVA injection in dialysis patients with CKD-aP in the U.S. under profit share agreements. We have partnered with VFMCRP to commercialize KORSUVA worldwide, excluding Japan (Maruishi/sub-licensee Kissei), and South Korea (CKDP). VFMCRP is a leading nephrology commercial organization with a significant presence in nephrology offices and dialysis centers. We are launching KORSUVA injection into a highly concentrated market. The dialysis market in the U.S. is dominated by two key providers, Fresenius and Davita, which combined control about 75% of the market. In addition, about 80% of the CKD hemodialysis patients are insured by Medicare.
Our U.S. commercial partner, Vifor Pharma Group, submitted the payment reimbursement application for TDAPA and the HCPCS to CMS in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years.
We have built a pipeline around an oral formulation of difelikefalin, the active compound in KORSUVA injection. We are developing Oral KORSUVA (difelikefalin) in programs to create potential opportunities across all three disease categories with chronic pruritus. This platform of Oral KORSUVA (difelikefalin) programs is designed to significantly expand the addressable market and patient populations that might benefit from our compound. We have four clinical programs in disease areas with about 16 million potential patients: NDD-CKD associated pruritus, AD, CLD, and NP.
Based on our completed Phase 2 trials and FDA End of Phase 2 meetings, in the first quarter of 2022, we plan to initiate two Phase 3 registrational programs of Oral KORSUVA (difelikefalin) for the treatment of pruritus, one in NDD-CKD and the other in AD.
In earlier-stage programs, we have a Phase 2 study ongoing for Oral KORSUVA (difelikefalin) in the treatment of NP, a neurologic pruritus in which chronic pruritus is the key manifestation of sensory neuropathic syndrome. This condition has no FDA-approved treatments nor robust data to support the use of any single therapy. We currently anticipate a readout on this trial in the second quarter of 2022. We believe this program could provide insight on Oral KORSUVA’s (difelikefalin) potential in other chronic neurologic pruritus conditions. In addition, we have an ongoing Phase 2 study of Oral KORSUVA (difelikefalin) for the treatment of PBC for which we currently anticipate a readout in
78
the second half of 2022. This program could provide insight into whether Oral KORSUVA (difelikefalin) has utility in other chronic liver diseases.
We were incorporated and commenced operations in 2004, and our primary activities to date have been organizing and staffing our company, developing our lead product and product candidates, including conducting preclinical studies and clinical trials of difelikefalin-based product candidates and raising capital. To date, we have financed our operations primarily through sales of our equity and debt securities and payments from license agreements. KORSUVA injection was approved in the U.S. in August 2021, with commercial launch expected in April 2022.
Recent Developments
COVID-19 Update
The extent of the impact of the ongoing COVID-19 pandemic on our business, operations and clinical development and regulatory timelines and plans remains uncertain, and will depend on certain developments, including the duration and outbreak and spread of variants and its impact on our clinical trial enrollment, trial sites, partners, CROs, third-party manufacturers, and other third parties with whom we do business, as well as its impact on regulatory authorities and our key scientific and management personnel. The timing of our submission of our NDA to the FDA for KORSUVA injection was not affected, as we submitted the NDA in December 2020. The COVID-19 pandemic, however, has affected, and may in the future affect, the initiation of certain trial sites and patient enrollment for our ongoing Phase 2 clinical trials of Oral KORSUVA (difelikefalin) for moderate-to-severe pruritus in patients with NP, and for the treatment of pruritus in patients with hepatic impairment due to PBC. While we currently do not expect any significant delays in our clinical development or commercial timelines, the ultimate impact of the evolving COVID-19 pandemic remains difficult to predict.
To the extent possible, we are conducting business as usual, with necessary or advisable modifications to employee travel and employee work locations. We are continuing to actively monitor the rapidly evolving situation related to COVID-19 and may take further actions that alter our operations, including those that may be required by federal, state or local authorities, or that we determine are in the best interests of our employees, partners and other third-parties with whom we do business. The extent to which the ongoing and evolving COVID-19 pandemic may affect our business, operations and clinical development and regulatory timelines and plans, including the resulting impact on our expenditures and capital needs, remains uncertain.
Vifor and VFMCRP Milestone Payments
In October 2021, after the expiration of the requisite waiting period under the HSR Act, we received a $50.0 million milestone payment from Vifor and issued 3,282,391 shares of our common stock in connection with U.S. regulatory approval of KORSUVA injection on August 23, 2021 (see Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations – Collaboration and License Agreements – Vifor (International) Ltd.).
Also in October 2021, we received a $15.0 million milestone payment from VFMCRP in connection with U.S. regulatory approval of KORSUVA injection on August 23, 2021 (see Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations – Collaboration and License Agreements – VFMCRP).
Christopher Posner Appointed as President and Chief Executive Officer
Christopher Posner was appointed as our President and CEO, effective November 9, 2021. Mr. Posner joins us from LEO Pharma, Inc., the U.S. affiliate of LEO Pharma A/S, a global leader in medical dermatology, where he was President and CEO. Mr. Posner succeeds Dr. Derek Chalmers, who transitioned to a Senior Advisor role to us.
79
Collaboration and License Agreements
Vifor (International) Ltd. (Vifor)
In October 2020, we entered into the Vifor Agreement under which we granted Vifor an exclusive license solely in the United States to use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA (difelikefalin) injection for all therapeutic uses relating to the inhibition, prevention or treatment of itch associated with pruritus in hemodialysis and peritoneal dialysis patients in the United States. Under the Vifor Agreement, we retain all rights with respect to the clinical development of, and activities to gain regulatory approvals of, KORSUVA (difelikefalin) injection in the United States.
Under the terms of the Vifor Agreement, we received from Vifor an upfront payment of $100.0 million and an additional payment of $50.0 million for the purchase of an aggregate of 2,939,552 shares of our common stock at a price of $17.0094 per share, which represents a premium over a pre-determined average closing price of our common stock. The purchase of our common stock was governed by the Vifor Stock Purchase Agreement.
After U.S. regulatory approval of KORSUVA injection in August 2021, we received an additional $50.0 million in October 2021 for the purchase of an aggregate of 3,282,391 shares of our common stock at a price of $15.23 per share, which represents a 20% premium to the 30-day trailing average price of our common stock. The purchase of our common stock was governed by the Vifor Stock Purchase Agreement. The excess of the stock purchase price over the cost of the purchased shares at the closing price of our common stock on the date of the achievement of the milestone of $5.0 million was included as license and milestone fees revenue for accounting purposes for the year ended December 31, 2021. In addition, pursuant to the Vifor Agreement, we are eligible to receive payments of up to $240.0 million upon the achievement of certain sales-based milestones (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
We retain the right to make and have made KORSUVA injection, on a non-exclusive basis, in the United States for commercial sale of KORSUVA injection for use in all therapeutic uses to prevent, inhibit or treat itch associated with pruritus in hemodialysis and peritoneal-dialysis patients anywhere in the world and for supply of Licensed Product to Vifor under the terms of a supply agreement, or the Vifor Supply Agreement, which was executed in September 2021. The supply price is our COGS, as calculated under GAAP, plus an agreed upon margin. The Vifor Supply Agreement will co-terminate with the Vifor Agreement.
The Vifor Agreement provides full commercialization rights in dialysis clinics to Vifor in the United States under a profit-sharing arrangement. Pursuant to the profit-sharing arrangement, we will generally be entitled to 60% of the net profits (as defined in the Vifor Agreement) from sales of KORSUVA injection in the United States (excluding sales to Fresenius Medical Center dialysis clinics, compensation for which is governed by the VFMCRP Agreement) and Vifor is entitled to 40% of such net profits, subject to potential temporary adjustment in future years based on certain conditions. Under the Vifor Agreement, in consideration of Vifor’s conduct of the marketing, promotion, selling and distribution of KORSUVA injection in the United States, we will pay a marketing and distribution fee to Vifor based on the level of annual net sales. This fee will be deducted from product sales in calculating the net profits that are subject to the profit-sharing arrangement under the Vifor Agreement.
The Vifor Agreement will continue in effect until its expiration upon the cessation of commercial sale of KORSUVA injection in the United States by Vifor and its affiliates and sublicensees, or until the earlier termination of the Vifor Agreement.
In connection with the Vifor Agreement, the parties entered into the Vifor Purchase Agreement, governing the issuance of our common stock to Vifor. Pursuant to the Vifor Purchase Agreement, Vifor will not, and will not cause any direct or indirect affiliate to, during the period beginning on October 15, 2020 and ending at the close of business on October 15, 2022, or the Restricted Period, (i) offer, pledge, sell, contract to sell, sell any option or contract to purchase, purchase any option or contract to sell, grant any option, right or warrant to purchase, lend, or otherwise transfer or dispose of, directly or indirectly, any shares of our common stock or any securities convertible into or exercisable or exchangeable for our common stock (including without limitation, common stock or such other securities
80
which may be deemed to be beneficially owned by Vifor in accordance with the rules and regulations of the SEC and securities which may be issued upon exercise of a stock option or warrant) owned by Vifor as of the date hereof or acquired prior to the end of the Restricted Period (collectively with the common stock, referred to as the Lock-Up Securities, except any such sale, option or contract by and between Vifor and one of its affiliates (including Vifor Pharma Group Ltd. or VFMCRP), (ii) enter into any hedging, swap or other agreement or transaction that transfers, in whole or in part, any of the economic consequences of ownership of the Lock-Up Securities, whether any such transaction described in clause (i) or (ii) above is to be settled by delivery of Lock-Up Securities, in cash or otherwise, (iii) make any demand for or exercise any right with respect to the registration of any Lock-Up Securities, or (iv) publicly disclose the intention to do any of the foregoing.
Under the Vifor Purchase Agreement, the parties also agreed that, in certain circumstances, upon the request of Vifor, the parties will enter into a registration rights agreement prior to the end of the Restricted Period that would provide Vifor (or its affiliate transferee) customary registration rights with respect to the shares of common stock issued pursuant to the stock purchase agreement following the expiration of the Restricted Period.
Vifor Fresenius Medical Care Renal Pharma Ltd. (VFMCRP)
In May 2018, we entered into the VFMCRP Agreement with VFMCRP, a joint venture between Vifor Pharma Group and Fresenius Medical Care, under which we granted VFMCRP a license to seek regulatory approval to commercialize, import, export, use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA (difelikefalin) injection for all therapeutic uses to prevent, inhibit or treat itch associated with pruritus in hemodialysis and peritoneal-dialysis patients worldwide (excluding the United States, Japan and South Korea). We retain full development and commercialization rights for KORSUVA injection for the treatment of CKD-aP in dialysis patients in the U.S. except in the dialysis clinics of Fresenius Medical Care North America, or FMCNA, where we and VFMCRP will promote KORSUVA injection under a profit-sharing arrangement.
Upon entry into the VFMCRP Agreement, VFMCRP made a non-refundable, non-creditable $50 million upfront payment to us and Vifor purchased 1,174,827 shares of our common stock for $20 million, at a premium for the price of $17.024 per share, which represented a premium over a pre-determined average closing price of our common stock. The purchase of our common stock was governed by a separate stock purchase agreement.
After U.S. regulatory approval of KORSUVA injection in August 2021, we received a $15.0 million regulatory milestone payment in October 2021, which was recorded as license and milestone fees revenue for the year ended December 31, 2021 (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
We are eligible to receive from VFMCRP additional regulatory and commercial milestone payments in the aggregate of up to $455.0 million, consisting of up to $15.0 million in regulatory milestones and up to $440.0 million in tiered commercial milestones, all of which are sales-related. We are also eligible to receive tiered double-digit royalty payments based on annual net sales, as defined, of KORSUVA (difelikefalin) injection in the licensed territories. In the United States, we and VFMCRP will promote KORSUVA (difelikefalin) injection in the dialysis clinics of FMCNA under a profit-sharing arrangement (subject to the terms and conditions of the VFMCRP Agreement) based on net FMCNA clinic sales recorded by us.
We retain the right to make and have made KORSUVA (difelikefalin) injection worldwide (excluding the United States, Japan and South Korea), or the Territory, for commercial sale by VFMCRP in or outside the Territory, and for supply of KORSUVA (difelikefalin) injection to VFMCRP under the terms of a supply agreement, or the VFMCRP Supply Agreement, which was executed in May 2020. The supply price is our COGS, as calculated under GAAP, plus an agreed upon margin. The VFMCRP Supply Agreement will co-terminate with the VFMCRP Agreement.
Maruishi Pharmaceutical Co., Ltd. (Maruishi)
In April 2013, we entered into a license agreement with Maruishi, or the Maruishi Agreement, under which we granted Maruishi an exclusive license to develop, manufacture and commercialize drug products containing difelikefalin
81
in Japan in the acute pain and uremic pruritus fields. Maruishi has a right of first negotiation for any other indications for which we develop difelikefalin and, under certain conditions, Maruishi may substitute another pruritus indication for the uremic pruritus indication originally included in its license from us. Maruishi is required to use commercially reasonable efforts, at its expense, to develop, obtain regulatory approval for and commercialize difelikefalin in Japan. We are required to use commercially reasonable efforts, at our expense, to develop, obtain regulatory approval for and commercialize difelikefalin in the United States.
In January 2022, Maruishi and its sublicensee Kissei confirmed the primary endpoint was achieved in a Japanese Phase 3 clinical study (double-blind, placebo-controlled period) of difelikefalin injection for the treatment of pruritus in hemodialysis patients. In the Phase 3 study, 178 patients were administered difelikefalin or placebo for 6 weeks followed by an open-label extension period of difelikefalin administration for 52 weeks. The primary endpoint, change in itch NRS score, and the secondary endpoint, change in itching scores of Shiratori severity criteria, were significantly improved from baseline compared to the placebo group. Difelikefalin was well-tolerated.
Under the terms of the Maruishi Agreement, we received a non-refundable and non-creditable upfront license fee of $15.0 million and are eligible to receive up to an aggregate of $10.5 million in clinical development and regulatory milestones (before contractual foreign currency exchange adjustments). In January 2021, we met the milestone criteria, as set forth in the Maruishi Agreement, for Maruishi’s first initiation of a Phase 3 trial for uremic pruritus in Japan. As a result, we received the $2.0 million milestone payment ($1.9 million after contractual foreign currency exchange adjustments) in May 2021. As of December 31, 2021, we have received $4.5 million (before contractual foreign currency exchange adjustments) of clinical development and regulatory milestones from Maruishi. We are also eligible to receive a one-time sales milestone of one billion Yen when a certain sales level is attained. We also receive a mid-double-digit percentage of all non-royalty payments received by Maruishi from its sublicensees, if any. We are also eligible to receive tiered royalties based on net sales, if any, with minimum royalty rates in the low double digits and maximum royalty rates in the low twenties. Maruishi’s obligation to pay us royalties continues, on a product-by-product basis, until the expiration of the last-to-expire licensed patent covering such product or the later expiration of any market exclusivity period.
The Maruishi Agreement continues until terminated. Either we or Maruishi may terminate the Maruishi Agreement for the other party’s breach of the agreement or bankruptcy. Maruishi may terminate the agreement at any time at will. We may terminate the agreement as a whole if Maruishi challenges the licensed patent rights, and we may terminate the agreement with respect to any indication if Maruishi discontinues its development activities. In addition, in connection with the Maruishi Agreement, Maruishi made an $8.0 million equity investment in our company.
Chong Kun Dang Pharmaceutical Corporation (CKDP)
In April 2012, we entered into a license agreement with CKDP, or the CKDP Agreement, under which we granted CKDP an exclusive license to develop, manufacture and commercialize drug products containing difelikefalin in South Korea. CKDP is required to use commercially reasonable efforts, at its expense, to develop, obtain regulatory approval for and commercialize difelikefalin in South Korea. We are required to use commercially reasonable efforts, at our expense, to develop, obtain regulatory approval for and commercialize difelikefalin in the United States.
Under the terms of the CKDP Agreement, we received a non-refundable and non-creditable $0.6 million upfront payment and are eligible to receive up to an aggregate of $3.8 million in development and regulatory milestones (before South Korean withholding taxes). During the year ended December 31, 2020, we received a milestone payment of $0.6 million (net of South Korean withholding tax) from CKDP, as set forth in the CKDP Agreement, for completion of a Phase 3 trial for uremic pruritus in the United States. As of December 31, 2021, we have received $2.3 million (before South Korean withholding tax) of development and regulatory milestones. We are also eligible to receive a mid-double-digit percentage of all non-royalty payments received by CKDP from its sublicensees, if any, and tiered royalties ranging from the high single digits to the high teens based on net sales, if any. CKDP’s obligation to pay us royalties continues, on a product-by-product basis, until the expiration of the last-to-expire licensed patent covering such product or the later expiration of any market exclusivity period.
82
The CKDP Agreement continues until CKDP no longer has any obligation to pay us royalties on any product. Either we or CKDP may terminate the CKDP Agreement for the other party’s breach of the CKDP Agreement or bankruptcy. CKDP may terminate the CKDP Agreement if any of the licensed patent rights is invalid, unenforceable, is narrowed in scope or is deemed unpatentable, except as a result of a challenge by CKDP, or a third party commercializes a product containing a compound identical to difelikefalin without infringing any of the licensed patent rights in South Korea. We may terminate the CKDP Agreement if CKDP challenges the licensed patent rights or if a third party in South Korea owns an issued patent that claims difelikefalin and CKDP’s sale of products would infringe that patent. In addition, in connection with the CKDP Agreement, CKDP made a $0.4 million equity investment in our company.
Manufacturing and License Agreements
Polypeptide Laboratories S.A. (PPL)
In July 2021, we entered into an API Commercial Supply Agreement with PPL that defines each party’s responsibilities with respect to PPL’s manufacture and supply of API for the difelikefalin injection product candidate. Under the API Commercial Supply Agreement, PPL shall manufacture API at its facility for sale and supply to us, in the amounts as set forth in purchase orders to be provided by us. We will be required to purchase our requirements of API for each year of the term of the agreement, based on internal forecasts.
The API Commercial Supply Agreement will continue until the fifth anniversary of the approval by the FDA of the new drug application for KORSUVA injection, unless the API Commercial Supply Agreement is earlier terminated, and will automatically be extended for successive five-year periods unless either party gives notice to the other party of its intention to terminate.
Enteris Biopharma, Inc. (Enteris)
In August 2019, we entered into the Enteris License Agreement with Enteris. Pursuant to the Enteris License Agreement, Enteris granted to us a non-exclusive, royalty-bearing license, including the right to grant sublicenses, under certain proprietary technology and patent rights related to or covering formulations for oral delivery of peptide active pharmaceutical ingredients with functional excipients to enhance permeability and/or solubility, known as Enteris’s Peptelligence® technology, to develop, manufacture and commercialize products using such technology worldwide, excluding Japan and South Korea.
As consideration for the licensed rights under the Enteris License Agreement, we paid an upfront fee equal to $8.0 million, consisting of $4.0 million in cash and $4.0 million in shares of our common stock pursuant to the Enteris Purchase Agreement described below. As a result, we recognized $8.0 million of R&D expense related to the Enteris License Agreement during the year ended December 31, 2019.
We are also obligated, pursuant to the Enteris License Agreement, to pay Enteris (1) milestone payments upon the achievement of certain development, regulatory and commercial milestones and (2) low-single digit royalty percentages on net sales of licensed products, subject to reductions in specified circumstances. Until the second anniversary of the entry into the Enteris License Agreement, we had the right, but not the obligation, to terminate our obligation to pay any royalties under the Enteris License Agreement in exchange for a lump sum payment in cash, or the Royalty Buyout. We did not exercise our Royalty Buyout right and such right expired in August 2021. During the years ended December 31, 2021 and 2020, we paid $15.0 million and $5.0 million, respectively, to Enteris for milestones earned in relation to the Enteris License Agreement, which were recorded in R&D expense for the respective periods.
The Enteris License Agreement will expire on a country-by-country, licensed product-by-licensed product basis upon the later of (1) the expiration (or invalidation) of all valid claims in licensed patent rights that cover such product in such country, (2) the end of the calendar quarter in which generic competition (as defined in the Enteris License Agreement) occurs for such product in such country and (3) ten years from the first commercial sale of such product.
Either party may terminate the Enteris License Agreement upon written notice if the other party has failed to remedy a material breach within 60 days (or 30 days in the case of a material breach of a payment obligation). Enteris
83
may terminate the Enteris License Agreement upon 30 days’ written notice to us if we or any of our affiliates formally challenge the validity of any licensed patent rights or assists a third party in doing so. We may terminate the Enteris License Agreement for any reason or no reason (a) prior to receipt of first regulatory approval for a licensed product in the United States for any indication upon 30 days’ prior written notice to Enteris or (b) on or after receipt of first regulatory approval for a licensed product in the United States for any indication upon 60 days’ prior written notice to Enteris.
In August 2019, in connection with the Enteris License Agreement, we entered into the Enteris Purchase Agreement with Enteris and its affiliate, EBP Holdco LLC, collectively referred to as Purchaser, pursuant to which we issued and sold to Purchaser 170,793 shares of our common stock in a private placement. Such shares were issued in satisfaction of the $4.0 million portion of the upfront fee payable in shares of our common stock pursuant to the Enteris License Agreement and for no additional consideration, based on a purchase price of $23.42 per share, which was equal to the 30-day volume weighted average price of our common stock on August 20, 2019. Pursuant to the Enteris Purchase Agreement, we effected the registration and sale of the shares issued and sold to Purchaser thereunder in accordance with the applicable requirements of the Securities Act of 1933, as amended, or the Securities Act, which included the filing of a registration statement with the SEC on September 9, 2019. In addition, the Purchase Agreement includes customary representations, warranties and covenants by us.
Patheon UK Limited (Patheon)
In July 2019, we entered into an MSA with Patheon. The MSA governs the general terms under which Patheon, or one of its affiliates, will provide non-exclusive manufacturing services to us for the drug products specified by us from time to time. Pursuant to the MSA, we have agreed to order from Patheon at least a certain percentage of our commercial requirements for a product under a related Product Agreement. Each Product Agreement that we may enter into from time to time will be governed by the terms of the MSA, unless expressly modified in such Product Agreement.
The MSA has an initial term ending December 31, 2023, and will automatically renew after the initial term for successive terms of two years each if there is a Product Agreement in effect, unless either party gives notice of its intention to terminate the MSA at least 18 months prior to the end of the then current term.
Either party may terminate the MSA or a Product Agreement upon written notice if the other party (1) has failed to remedy a material breach within a specified time or (2) is declared insolvent or bankrupt, voluntarily files a petition of bankruptcy or assigns such agreement for the benefit of creditors. We may terminate a Product Agreement (a) upon 90 days’ prior written notice if any governmental agency takes any action that prevents us from selling the relevant product in the relevant territory, (b) upon six months’ prior written notice if we do not intend to order manufacturing services due to a product’s discontinuance in the market, or (c) upon 90 days’ prior written notice if we determine that the manufacture or supply of a product likely infringes third-party rights. Patheon may terminate the MSA or a Product Agreement (i) upon six months’ prior written notice if we assign such agreement to an assignee that is unacceptable to Patheon for certain reasons, or (ii) upon 30 days’ prior written notice if, after the first year of commercial sales, we forecast zero volume for 12 months.
The MSA contains, among other provisions, customary representations and warranties by the parties, a grant to Patheon of certain limited license rights to our intellectual property in connection with Patheon’s performance of the services under the MSA, certain indemnification rights in favor of both parties, limitations of liability and customary confidentiality provisions.
Also in July 2019, we entered into two related Product Agreements under the MSA, one with each of Patheon and Patheon Greenville, to govern the terms and conditions of the manufacture of commercial supplies of difelikefalin injection, our lead product candidate. Pursuant to the Product Agreements, Patheon and Patheon Greenville will manufacture commercial supplies of difelikefalin injection at the Monza, Italy and Greenville, North Carolina manufacturing sites, respectively, from API supplied by us. Patheon and Patheon Greenville will be responsible for supplying the other required raw materials and packaging components, and will also provide supportive manufacturing services such as quality control testing for raw materials, packaging components and finished product.
84
Components of Operating Results
Revenue
Substantially all of our revenue recognized to date has consisted of upfront and milestone payments under license agreements with Vifor, VFMCRP, Maruishi and CKDP, some or all of which was deferred upon receipt, sub-license payments under our license agreement with Maruishi for difelikefalin, as well as license agreements for CR665, our first-generation drug program for which development efforts have ceased, clinical compound sales from certain license agreements, and commercial supply revenue from Vifor in 2021. Through December 31, 2021, we have earned a total of $74.7 million in clinical development or regulatory milestone payments (including the $50.0 million equity investment from Vifor and $15.0 million milestone payment from VFMCRP for the U.S. regulatory approval of KORSUVA injection in August 2021) and clinical compound and commercial sales from certain license agreements. Of the $50.0 million equity milestone, $5.0 million, representing the premium of the purchase price over the market price of our common stock, was recognized as revenue during the year ended December 31, 2021. We have not yet received any royalties under any of our collaborations.
We and Vifor began commercializing KORSUVA injection in the U.S. in December 2021 and we expect commercial launch of KORSUVA injection in April 2022 and associated revenues in the second quarter of 2022.
Revenue from sales of KORSUVA injection in future periods is subject to uncertainties and will depend on several factors, including the success of our and our commercial partners’ commercialization efforts in the U.S., the number of new patients switching to KORSUVA injection, patient retention and demand, the number of physicians prescribing KORSUVA injection, the rate of monthly prescriptions, reimbursement from third-party payors, the conversion of patients from our clinical trials to commercial customers, and market trends. More specifically, in December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years. CMS expressed in its written communication to us and Vifor Pharma, a continuing interest in engaging with the companies regarding potential post-TDAPA support to ensure all beneficiaries with ESRD have access to innovative products such as KORSUVA injection. However, there is no assurance that KORSUVA injection will be able to maintain its price established in the TDAPA period in the post-TDAPA timeframe, which could significantly impact our revenues in future periods. We will continue to monitor and analyze this data during the initial launch period in 2022.
Cost of Goods Sold (COGS)
COGS includes costs related to sales of our commercial product, KORSUVA injection, to Vifor. Costs related to the sales of KORSUVA injection are generally recognized upon receipt of shipment by Vifor. Our COGS for KORSUVA injection includes the cost of producing commercial product that correspond with commercial supply revenue, such as third-party supply and overhead costs, as well as certain period costs related to freight, packaging, stability, and quality testing. We expect our COGS to increase as Vifor generates additional sales of KORSUVA injection in the future.
Research and Development (R&D)
Our R&D expenses relate primarily to the development of difelikefalin. R&D expenses consist of expenses incurred in performing R&D activities, including compensation and benefits for full-time R&D employees, clinical trial and related clinical manufacturing expenses, third-party formulation expenses or milestone payments, fees paid to CROs and other consultants, stock-based compensation for R&D employees and consultants, and other outside expenses. Our R&D expenses also included expenses related to preclinical activities for our earlier stage programs in prior periods and may include such expenses in the future.
R&D costs are expensed as incurred. Non-refundable advance payments for goods or services to be received in the future for use in R&D activities are deferred and capitalized. The capitalized amounts are expensed as the related goods are delivered or the services are performed. Most of our R&D costs have been external costs, which we track on a
85
program-by program basis. Our internal R&D costs are primarily compensation expenses for our full-time R&D employees. We do not track internal R&D costs on a program-by-program basis.
R&D activities are central to our business model. Product candidates in later stages of clinical development generally have higher development costs than those in earlier stages of clinical development, primarily due to the increased size and duration of later-stage clinical trials. Based on our current development plans, we presently expect that our R&D expenses for 2022 will be higher than 2021. However, it is difficult to determine with certainty the duration and completion costs of our current or future nonclinical programs and clinical trials of our product candidates, or if, when or to what extent we will generate revenues from the commercialization and sale of any of our product candidates that obtain regulatory approval. We may never succeed in achieving regulatory approval for any of our product candidates.
The duration, costs and timing of clinical trials and development of our product candidates will depend on a variety of factors including, but not limited to:
| ● | per patient trial costs; |
| ● | the number of patients that participate in the trials; |
| ● | the number of sites included in the trials; |
| ● | the countries in which the trial is conducted; |
| ● | the length of time required to enroll eligible patients; |
| ● | the number of doses that patients receive; |
| ● | the drop-out or discontinuation rates of patients; |
| ● | potential additional safety monitoring or other studies requested by regulatory agencies; |
| ● | the duration of patient follow-up; and |
| ● | the efficacy and safety profile of the product candidate. |
In addition, the probability of success for each product candidate will depend on numerous factors, including competition, manufacturing capability and commercial viability. We will determine which programs to pursue and how much to fund each program in response to the scientific and clinical success of each product candidate, as well as an assessment of each product candidate’s commercial potential.
General and Administrative (G&A)
G&A expenses consist primarily of salaries and other related costs, including stock-based compensation, for personnel in executive, finance, accounting, legal, business development, information technology, or IT, and human resources functions. Other costs include facility costs not otherwise included in R&D expenses, legal fees, insurance costs, investor relations costs, patent costs and fees for accounting and consulting services.
We anticipate that our G&A expenses for 2022 will be consistent with 2021 to support our continued R&D activities and for our product candidates. These expenses will likely include costs related to the hiring of additional personnel, fees to outside consultants, lawyers, accountants and investor relations firms. In addition, if Oral KORSUVA (difelikefalin) or any future product candidate obtains regulatory approval for marketing, we expect to incur expenses associated with building a sales and marketing team.
86
Our license agreement with Vifor provides full commercialization rights of KORSUVA injection to Vifor under a profit-sharing arrangement. Under this profit-sharing arrangement, in consideration of Vifor’s conduct of the marketing, promotion, selling and distribution of KORSUVA injection in the U.S., we will pay a marketing and distribution fee to Vifor based on the level of annual net sales. This fee will be deducted from product sales in calculating the net profits that are subject to the profit-sharing arrangement (see Note 12 of Notes to Financial Statements, Collaboration and Licensing Arrangements, in this Annual Report on Form 10-K).
Other Income, Net
Other income, net consists of interest and dividend income earned primarily on our cash, cash equivalents, and marketable securities, realized gains and losses on the sale of marketable securities and property and equipment as well as accretion of discounts/amortization of premiums on purchases of marketable securities. In the event we record a credit loss expense on our available-for-sale debt securities, those expenses would be offset against other income.
Benefit from Income Taxes
The benefit from income taxes relates to state R&D tax credits exchanged for cash pursuant to the Connecticut R&D Tax Credit Exchange Program, which permits qualified small businesses engaged in R&D activities within Connecticut to exchange their unused R&D tax credits for a cash amount equal to 65% of the value of the exchanged credits. Because our revenue in 2020 exceeded $70.0 million, we are not eligible to exchange our 2021 R&D tax credit for cash, therefore there was no benefit from income taxes for the year ended December 31, 2021.
Results of Operations
Comparison of the years ended December 31, 2021, 2020 and 2019
Revenue
Year Ended December 31, | |||||||||||||
| 2021 |
|
| 2020 |
|
| 2019 | ||||||
Dollar amounts in thousands | |||||||||||||
% change | % change | ||||||||||||
License and milestone fees | $ | 21,223 | (84) | % | $ | 134,439 | 581 | % | $ | 19,746 | |||
Collaborative revenue |
| 706 |
| N/A | % |
| — |
| — | % |
| — | |
Commercial supply revenue | 701 | N/A | % | — | — | % | — | ||||||
Clinical compound revenue |
| 398 |
| (38) | % |
| 643 |
| 359 | % |
| 140 | |
Total revenue | $ | 23,028 |
| (83) | % | $ | 135,082 |
| 579 | % | $ | 19,886 | |
License and milestone fee revenue
License and milestone fees revenue of $21.2 million for the year ended December 31, 2021 was related to milestone payments of $20.0 million we earned from Vifor and VFMCRP that was allocated to the license fee performance obligation under the Vifor and VFMCRP agreements, as the variable consideration was deemed probable upon the regulatory approval of KORSUVA injection in August 2021, and a milestone payment of $1.2 million that we earned in January 2021 from Maruishi’s first initiation of a Phase 3 trial for uremic pruritus in Japan that was allocated to the license fee performance obligation under the Maruishi Agreement (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
License and milestone fees revenue of $134.4 million for the year ended December 31, 2020 was related to license fees of $111.6 million earned by us in connection with the Vifor Agreement that we entered into in October 2020, license fees of $22.3 million earned by us in connection with the VFMCRP Agreement, and $0.6 million (net of South Korean withholding taxes) earned by us for achieving a development milestone under the CKDP Agreement (see
87
Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
License and milestone fees revenue of $19.7 million for the year ended December 31, 2019 was related to license fees earned by us during the period in connection with the VFMCRP Agreement (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
Collaborative Revenue
Collaborative revenue of $706,000 for the year ended December 31, 2021 was related to the milestone payment we earned in January 2021 from Maruishi’s first initiation of a Phase 3 trial for uremic pruritus in Japan that was allocated to the R&D services performance obligation under the Maruishi Agreement. There were no collaborative revenues for each of the years ended December 31, 2020 and 2019 (see Notes 12 and 13 of Notes to Financial Statements, Collaboration and Licensing Agreements and Revenue Recognition, respectively, in this Annual Report on Form 10-K).
Commercial Supply Revenue
Commercial supply revenue of $701,000 for the year ended December 31, 2021 was related to sales of KORSUVA injection to Vifor. We and Vifor began commercializing KORSUVA injection in the U.S. in December 2021 and anticipate commercial launch in April 2022.
Clinical compound revenue
Clinical compound revenue of $398,000 for the year ended December 31, 2021 was related to the sale of clinical compound to VFMCRP for $361,000 and to Maruishi for $37,000. Clinical compound revenue of $643,000 for the year ended December 31, 2020 was related to the sales of clinical compound to VFMCRP for $115,000 and to Maruishi for $528,000. Clinical compound revenue of $140,000 for the year ended December 31, 2019 was related to the sale of clinical compound to Maruishi.
Cost of Goods Sold (COGS)
For the year ended December 31, 2021, no COGS was recognized as all inventory costs for KORSUVA injection prior to regulatory approval on August 23, 2021 were expensed as incurred (see Note 2 of Notes to Financial Statements, Summary of Significant Accounting Policies – Inventories and Cost of Goods Sold (COGS), in this Annual Report on Form 10-K).
Research and Development (R&D) Expense
Year Ended December 31, | |||||||||||||
2021 | 2020 | 2019 | |||||||||||
Dollar amounts in thousands | |||||||||||||
% change | % change | ||||||||||||
Direct clinical trial costs | $ | 31,261 | (55) | % | $ | 68,937 | (14) | % | $ | 80,098 | |||
Consultant services in support of clinical trials |
| 4,708 |
| (19) | % |
| 5,792 |
| 30 | % |
| 4,470 | |
Stock-based compensation |
| 8,327 |
| 2 | % |
| 8,197 |
| 41 | % |
| 5,809 | |
Depreciation and amortization |
| 123 |
| 10 | % |
| 112 |
| 2 | % |
| 110 | |
Other R&D operating expenses |
| 38,282 |
| 54 | % |
| 24,813 |
| 6 | % |
| 23,333 | |
Total R&D expense | $ | 82,701 |
| (23) | % | $ | 107,851 |
| (5) | % | $ | 113,820 | |
For the year ended December 31, 2021 compared to the year ended December 31, 2020, the net decrease in direct clinical trial costs and related consultant costs primarily resulted from decreases totaling $40.3 million, mainly from activities related to the KALM-2 Phase 3 efficacy trial of KORSUVA injection in CKD patients undergoing hemodialysis, the Phase 3 (up to 12 weeks) safety trial of KORSUVA injection in CKD patients undergoing
88
hemodialysis, the KALM-1 Phase 3 efficacy trial and the 52-week open-label extension study of KORSUVA injection in CKD patients undergoing hemodialysis, the Phase 2 efficacy trial for pruritus associated with AD-aP, the Phase 2 efficacy trial of Oral KORSUVA (difelikefalin) in CKD-aP patients, costs associated with supportive Phase 1 studies, and costs associated with preparing for our NDA submission. There was also a decrease of $4.8 million in clinical and commercial drug manufacturing costs. These decreases were partially offset by an increase of $6.4 million, mainly from the Phase 2 efficacy and safety trial for pruritus associated with NP, start-up costs related to Oral CKD Phase 3 programs in non-hemodialysis patients, and other general costs. The increase in stock-based compensation expense was primarily related to additional stock option and time-based restricted stock unit grants to new and existing employees, partially offset by lower stock-based compensation expense associated with the vesting of performance-based restricted stock units during the year ended December 31, 2021, as compared to the comparable period in 2020. The increase in other R&D operating expenses primarily resulted from $15.0 million in milestones earned by Enteris during the year ended December 31, 2021 as compared to $5.0 million during the year ended December 31, 2020, and increases in payroll and related costs.
For the year ended December 31, 2020 compared to the year ended December 31, 2019, the net decrease in direct clinical trial costs and related consultant costs primarily resulted from decreases totaling $33.2 million, mainly from activities related to the KALM-1 Phase 3 efficacy trial and the 52-week open-label extension study of KORSUVA injection in CKD patients undergoing hemodialysis, the Phase 2 efficacy trial of Oral KORSUVA (difelikefalin) in CKD-aP patients, the KALM-2 Phase 3 efficacy trial of KORSUVA injection in CKD patients undergoing hemodialysis, the Phase 2 efficacy trial for CLD-aP, costs associated with a supportive Phase 1 study and other license fees. Those costs were partially offset by an increase of $19.4 million, mainly from the Phase 2 efficacy trial for pruritus associated with AD, the Phase 2 efficacy and safety trial for pruritus associated with NP, costs associated with a supportive Phase 1 study, costs associated with the preparation our NDA submission and other general costs. There was also an increase of $4.1 million in clinical and commercial drug manufacturing costs. The increase in stock-based compensation expense was primarily the result of additional stock option and restricted stock unit grants to new and existing employees, as well as additional stock-based compensation expense relating to the vesting of performance-based restricted stock units that were achieved in 2020 as compared to 2019 by certain executives. The increase in other R&D operating expenses primarily resulted from a $5.0 million milestone earned by Enteris during the year ended December 31, 2020, as well as increases in payroll and related costs and cost of clinical compound sales, partially offset by the upfront payment of $8.0 million made to Enteris upon entering the Enteris License Agreement during the year ended December 31, 2019 and decreases in travel and related costs.
The following table summarizes our R&D expenses by product candidate for the years ended December 31, 2021, 2020 and 2019:
Year Ended December 31, | ||||||||||||
2021 |
|
| 2020 |
|
| 2019 | ||||||
Dollar amounts in thousands | ||||||||||||
| % change |
|
| % change |
| |||||||
External research and development expenses: | ||||||||||||
KORSUVA (difelikefalin) injection - Pruritus | $ | 9,736 |
| (78) | % | $ | 44,026 |
| (26) | % | $ | 59,687 |
Oral KORSUVA (difelikefalin) - Pruritus |
| 25,761 |
| (16) | % |
| 30,491 |
| 25 | % |
| 24,475 |
Other |
| 18 |
| (85) | % |
| 123 |
| (70) | % |
| 406 |
Internal research and development expenses/milestone payments1 |
| 47,186 |
| 42 | % |
| 33,211 |
| 14 | % |
| 29,252 |
Total research and development expenses | $ | 82,701 |
| (23) | % | $ | 107,851 |
| (5) | % | $ | 113,820 |
_______________________________
1 Includes milestone payments of $15.0 million and $5.0 million to Enteris for the years ended December 31, 2021 and 2020, respectively.
89
General and Administrative (G&A) Expense
Year Ended December 31, | ||||||||||||
2021 | 2020 | 2019 | ||||||||||
Dollar amounts in thousands | ||||||||||||
| % change |
|
| % change |
| |||||||
Professional fees and public/investor relations | $ | 4,642 | 21 | % | $ | 3,841 | (1) | % | $ | 3,883 | ||
Stock-based compensation |
| 12,459 |
| 88 | % |
| 6,638 |
| (2) | % |
| 6,759 |
Depreciation and amortization |
| 125 |
| 29 | % |
| 97 |
| 11 | % |
| 88 |
Other G&A operating expenses |
| 12,184 |
| 8 | % |
| 11,270 |
| 61 | % |
| 7,015 |
Total G&A expense | $ | 29,410 |
| 35 | % | $ | 21,846 |
| 23 | % | $ | 17,745 |
For the year ended December 31, 2021 compared to the year ended December 31, 2020, the increase in professional fees and public/investor relations expenses was primarily the result of an increase in legal fees, partially offset by a decrease in consultants’ costs. The increase in stock-based compensation expense was primarily related to the modification of our former CEO’s stock option and time-based restricted stock unit awards in November 2021 resulting in additional compensation expense of approximately $5.1 million in 2021, additional time-based restricted stock unit grants to existing employees, and higher stock-based compensation expense associated with the vesting of performance-based restricted stock units during the year ended December 31, 2021, as compared to the comparable period in 2020. The increase in other G&A operating expenses was primarily the result of increases in payroll and related costs and insurance costs, partially offset by a decrease in commercial costs.
For the year ended December 31, 2020 compared to the year ended December 31, 2019, the decrease in professional fees and public/investor relations expenses was primarily the result of a decrease in consultants’ costs, partially offset by increases in accounting fees. The decrease in stock-based compensation expense was primarily the result of the resignation of our former Chief Financial Officer, or CFO, in December 2019, a decrease in stock-based compensation expense due to fewer performance-based restricted stock units vesting during 2020 as compared to 2019, and the issuance of common stock relating to the consulting agreement that ended in 2019, partially offset by additional stock option grants and restricted stock unit grants to employees and members of our Board of Directors, including our current CFO beginning in October 2020. The increase in other G&A operating expenses was primarily the result of increases in commercial costs, insurance costs, and payroll and related costs.
Other Income, Net
Year Ended December 31, | ||||||||||||
2021 |
|
| 2020 |
|
| 2019 | ||||||
Dollar amounts in thousands | ||||||||||||
% change | % change | |||||||||||
Other income, net | $ | 642 | (72) | % | $ | 2,334 | (48) | % | $ | 4,490 | ||
For the year ended December 31, 2021 compared to the year ended December 31, 2020, the decrease in other income, net was primarily due to an increase in net amortization expense of available-for-sale marketable securities and a decrease in interest income resulting from a lower yield on our portfolio of investments in the 2021 period.
For the year ended December 31, 2020 compared to the year ended December 31, 2019, the decrease in other income, net was primarily due to a decrease in net accretion income and a decrease in interest income resulting from a lower yield on our portfolio of investments in the 2020 period, partially offset by a realized gain of approximately $0.3 million from the sale of our available-for-sale marketable securities in the 2020 period.
We reviewed our available-for-sale debt securities as of December 31, 2021 and 2020 and determined that no credit loss expense was necessary as a result of unrealized losses on various securities not being considered material individually or in aggregate, and we expect that the cost basis of these available-for-sale securities is recoverable. We do not expect that unrealized losses on our available-for-sale debt securities will impact our liquidity in the short-term or long-term since our investments all mature at various dates through November 2024 based on capital requirements, and
90
it is not more likely than not that we will be required to sell these investments before recovery of their amortized cost bases.
Benefit from Income Taxes
For the years ended December 31, 2021, 2020 and 2019, pre-tax (losses) income were $(88.4) million, $7.7 million and $(107.2) million, respectively, and we recognized a benefit from income taxes of $691,000 and $816,000 for the years ended December 31, 2020 and 2019, respectively. Because our revenue in 2020 exceeded $70.0 million, we are not eligible to exchange our 2021 R&D tax credit for cash, therefore there was no benefit from income taxes for the year ended December 31, 2021.
The benefit from income taxes relates to state R&D tax credits exchanged for cash pursuant to the Connecticut R&D Tax Credit Exchange Program, as discussed above. We recognized a full valuation allowance against deferred tax assets at December 31, 2021, 2020 and 2019.
Cash Requirements, Liquidity, and Capital Resources
Short-Term and Long-Term Cash Requirements
Our primary uses of capital have been, and we expect will continue to be, compensation and related expenses, third-party clinical R&D services, and clinical costs related to the Oral KORSUVA (difelikefalin) program.
As of December 31, 2021, we have no commitments for capital expenditures in either the short-term or long-term. The following discussion summarizes our current and long-term material cash requirements as of December 31, 2021, which we expect to fund primarily with current unrestricted cash and cash equivalents and available-for-sale marketable securities:
Material Cash Requirements | |||||||||
| Total |
| Less than 1 Year |
| 1-2 Years | ||||
Operating lease obligations(1) | $ | 3,948 |
| $ | 1,957 | $ | 1,991 | ||
Manufacturing purchase obligations(2) | 3,794 |
| 3,794 | — | |||||
Other obligations(3) | 408 | — | 408 | ||||||
Total | $ | 8,150 | $ | 5,751 | $ | 2,399 | |||
| (1) | Operating lease obligations relate to our Stamford operating leases entered into in December 2015 and amended in June 2020 and continue through December 2023. See Note 18 of Notes to Financial Statements, Commitments and Contingencies, in this Annual Report on Form 10-K for details about our operating lease obligations. |
| (2) | Based on our MSA with Patheon that we entered into in July 2019, we have a purchase capacity reservation through 2022. We expect the majority of this capacity reservation will be reimbursed in accordance with the supply agreement with Vifor. See Note 18 of Notes to Financial Statements, Commitments and Contingencies, in this Annual Report on Form 10-K for details about our MSA with Patheon. We have no other material non-cancelable purchase commitments with any other contract manufacturers or service providers, as we have generally contracted on a cancelable purchase order basis. |
| (3) | We are required to maintain a stand-by letter of credit as a security deposit under our leases for office space in Stamford, Connecticut. See Note 8 of Notes to Financial Statements, Restricted Cash, in this Annual Report on Form 10-K for details about our letter of credit associated with our Stamford operating leases. |
As we anticipate revenue increasing in the short-term and long-term with the commercialization of KORSUVA injection, our costs of manufacturing will also increase.
Based on the Enteris License Agreement that we entered into in August 2019, we are obligated to pay (1) milestone payments upon the achievement of certain development, regulatory and commercial milestones and (2) low-single digit royalty percentages on net sales of licensed products, subject to reductions in specified circumstances. As
91
these milestone payments may or may not be achieved, and royalties may or may not be owed depending on our future commercial success, there were no future payments that were considered cash requirements in the table above as of December 31, 2021. See Note 18 of Notes to Financial Statements, Commitments and Contingencies, in this Annual Report on Form 10-K for details about our Enteris License Agreement.
We do not have any other requirements or off-balance sheet arrangements that have or are reasonably likely to have a material current or future effect on our financial condition, changes in financial condition, revenues or expenses, results of operations, liquidity, cash requirements or capital resources.
Since inception, we have incurred significant operating and net losses. We incurred net losses of $88.4 million and $106.4 million for the years ended December 31, 2021 and 2019, respectively. As of December 31, 2021, we had an accumulated deficit of $480.8 million. Although we generated net income for the year ended December 31, 2020 as a result of a commercial license transaction, we expect to continue to incur long-term significant expenses and operating and net losses in the foreseeable future, as we and our partner Vifor Pharma prepare for the commercial launch of KORSUVA injection and to develop and seek marketing approval for Oral KORSUVA (difelikefalin). However, we will not incur any material commercial costs on KORSUVA injection due to the licensing agreement with Vifor. Our financial results may fluctuate significantly from quarter to quarter and year to year, depending on the success of our commercialization efforts, timing of our clinical trials, the receipt of additional milestone payments, if any, under our licensing and collaborations with Vifor, VFMCRP, Maruishi and CKDP, the receipt of payments under any future collaborations and/or licensing agreements we may enter into, and our expenditures on other R&D activities.
We anticipate that our expenses will increase as we:
| ● | continue the development of Oral KORSUVA (difelikefalin) for AD-aP, NDD-CKD, CLD-PBC and NP; |
| ● | seek regulatory approvals for any product candidates that successfully complete clinical trials; |
| ● | establish a sales, marketing and distribution infrastructure and scale up external manufacturing capabilities to commercialize any other products for which we may obtain regulatory approval; |
| ● | maintain, expand and protect our global intellectual property portfolio; |
| ● | hire additional clinical, quality control and scientific personnel; and |
| ● | add operational, financial and management information systems and personnel, including personnel to support our drug development and potential future commercialization efforts. |
The successful commercialization of KORSUVA injection and the successful development of any of our other product candidates is highly uncertain. As such, at this time, we cannot reasonably estimate or know the nature, timing and costs of the efforts that will be necessary to successfully commercialize KORSUVA injection, complete the development of I.V. difelikefalin, oral difelikefalin or our other current and future programs. We are also unable to predict when, if ever, we will generate any further material net cash inflows from difelikefalin. This is due to the numerous risks and uncertainties associated with developing medicines, including the uncertainty of:
| ● | successful enrollment in, and completion of clinical trials; |
| ● | receipt of marketing approvals from applicable regulatory authorities; |
| ● | establishing commercial manufacturing capabilities or making arrangements with third-party manufacturers; |
| ● | obtaining and maintaining patent and trade secret protection and regulatory exclusivity for our product candidates; |
92
| ● | launching commercial sales of the products, if and when approved, whether alone or in collaboration with others; |
| ● | achieving meaningful penetration in the markets which we seek to serve; and |
| ● | obtaining adequate coverage or reimbursement by third parties, such as commercial payers and government healthcare programs, including Medicare and Medicaid. |
A change in the outcome of any of these variables with respect to the development of I.V. difelikefalin, oral difelikefalin or any of our future product candidates would significantly change the costs and timing associated with the development of that product candidate. Further, the timing of any of the above may be impacted by the ongoing COVID-19 pandemic, introducing additional uncertainty.
Although we and Vifor began commercializing KORSUVA injection in the U.S. in December 2021 and we expect commercial launch of KORSUVA injection in April 2022, and our other product candidates are still in clinical development and the outcome of these efforts is uncertain, we cannot estimate the actual amounts necessary to successfully complete the commercialization of KORSUVA injection and the development and commercialization of our other product candidates or whether, or when, we may achieve profitability. Until such time, if ever, as we can generate substantial product revenues, we expect to finance our cash needs through a combination of equity or debt financings and collaboration arrangements, including our existing licensing and collaboration agreements with Vifor, VFMCRP, Maruishi and CKDP.
We will require additional capital beyond our current balances of cash and cash equivalents and available-for-sale marketable securities and anticipated amounts as described above, and this additional capital may not be available when needed, on reasonable terms, or at all, and our ability to raise additional capital may be adversely impacted by potential worsening global economic conditions and the continuing disruptions to and volatility in the credit and financial markets in the United States and worldwide resulting from the ongoing COVID-19 pandemic and its variants. If we are not able to do so, we could be required to postpone, scale back or eliminate some, or all, of these objectives. To the extent that we raise additional capital through the future sale of equity or convertible debt, the ownership interest of our stockholders will be diluted, and the terms of these securities may include liquidation or other preferences that adversely affect the rights of our existing common stockholders. If we raise additional funds through the issuance of debt securities, these securities could contain covenants that would restrict our operations. If we raise additional funds through collaboration arrangements in the future, we may have to relinquish valuable rights to our technologies, future revenue streams or product candidates or grant licenses on terms that may not be favorable to us. If we are unable to raise additional funds through equity or debt financings when needed, we may be required to delay, limit, reduce or terminate our drug development or future commercialization efforts or grant rights to develop and market product candidates that we would otherwise prefer to develop and market ourselves.
Sources of Liquidity
Since our inception to date, we have raised an aggregate of $842.5 million to fund our operations, including (1) net proceeds of $446.3 million from the sale of shares of our common stock in five public offerings, including our initial public offering; (2) proceeds of $73.3 million from the sale of shares of our convertible preferred stock and from debt financings prior to our initial public offering; (3) payments of $224.9 million under our license and supply agreements, primarily with Vifor, VFMCRP, Maruishi, CKDP and an earlier product candidate for which development efforts ceased in 2007; and (4) net proceeds of $98.0 million from the purchase of our common stock in relation to the license agreements with Vifor and VFMCRP (see Note 12 of Notes to Financial Statements, Collaboration and Licensing Agreements, in this Annual Report on Form 10-K).
In order to fund our future operations, including our planned clinical trials, on March 1, 2022, we filed a universal shelf registration statement, or the Shelf Registration Statement, which provides for aggregate offerings of up to $300.0 million of common stock, preferred stock, debt securities, warrants or any combination thereof. The Shelf Registration Statement has not yet been declared effective by the Securities and Exchange Commission. The securities registered under the Shelf Registration Statement include $154.5 million of unsold securities that had been registered under our
93
previous Registration Statement on Form S-3 (File No. 333-230333) that was declared effective on April 4, 2019. We believe that our Shelf Registration Statement, once effective, will provide us with the flexibility to raise additional capital to finance our operations as needed.
We may offer additional securities under our Shelf Registration Statement, when declared effective, from time to time in response to market conditions or other circumstances if we believe such a plan of financing is in the best interests of our stockholders. On March 1, 2022, we entered into an open market sales agreement, or the Sales Agreement, with Jefferies LLC, as sales agent, pursuant to which we may, subject to the effectiveness of the Shelf Registration Statement, from time to time, issue and sell common stock with an aggregate value of up to $80.0 million in an at-the-market offering. Jefferies is acting as sole sales agent for any sales made under the Sales Agreement for a 3% commission on gross proceeds. The common stock will be sold at prevailing market prices at the time of the sale, and, as a result, prices may vary. Unless otherwise terminated earlier, the Sales Agreement continues until all shares available under the Sales Agreement have been sold.
As of December 31, 2021, we had $236.8 million in unrestricted cash and cash equivalents and available-for-sale marketable securities. We believe our current unrestricted cash and cash equivalents and available-for-sale marketable securities will be sufficient to fund our currently anticipated operating expenses and capital requirements through 2023, without giving effect to any additional potential milestone payments or potential product revenue we may receive under our licensing and collaboration agreements with Vifor, VFMCRP, Maruishi and CKDP. Our anticipated operating expenses include contractually committed costs as well as non-contractually committed clinical trial costs for trials that may be delayed or not initiated and other non-committed controllable costs.
Under the Vifor Agreement, we are eligible to receive commercial milestone payments in the aggregate of up to $240.0 million upon the achievement of certain sales-based milestones. In October 2021, we received a $50.0 million milestone payment from Vifor in exchange for the issuance of 3,282,391 shares of our common stock to Vifor as a result of the regulatory approval of KORSUVA injection in August 2021. As of December 31, 2021, we have received $50.0 million of regulatory milestones from Vifor.
Under the VFMCRP Agreement, we are eligible to receive additional regulatory and commercial milestone payments in the aggregate of up to $455.0 million, consisting of up to $15.0 million in regulatory milestones and up to $440.0 million in tiered commercial milestones, all of which are sales-related. We are also eligible to receive tiered double-digit royalty payments based on annual net sales, as defined in the VFMCRP Agreement, of difelikefalin injection in the licensed territories. In October 2021, we received a $15.0 million milestone payment from VFMCRP as a result of the regulatory approval of KORSUVA injection in August 2021. As of December 31, 2021, we have received $15.0 million of regulatory milestones from VFMCRP.
Under the Maruishi Agreement, we are also potentially eligible to earn up to an aggregate of $6.0 million in clinical development milestones and $4.5 million in regulatory milestones, before any foreign exchange adjustment, as well as tiered royalties, with percentages ranging from the low double digits to the low twenties, based on net sales of products containing difelikefalin in Japan, if any, and share in any sub-license fees. As of December 31, 2020, we have received milestone payments of $2.5 million before contractual foreign currency exchange adjustments under the Maruishi Agreement. In May 2021, we received a $2.0 million milestone payment ($1.9 million after contractual foreign currency exchange adjustments) for Maruishi’s first initiation of a Phase 3 trial for uremic pruritus in Japan in January 2021. As of December 31, 2021, we have received $4.5 million (before contractual foreign currency exchange adjustments) of clinical development and regulatory milestone from Maruishi.
Under the CKDP Agreement, we are potentially eligible to earn up to an aggregate of $2.3 million in clinical development milestones and $1.5 million in regulatory milestones, before South Korean withholding tax, as well as tiered royalties with percentages ranging from the high single digits to the high teens, based on net sales of products containing difelikefalin in South Korea, if any, and share in any sub-license fees. During the year ended December 31, 2020, we received $0.6 million (net of South Korean withholding tax) relating to a milestone payment received from CKDP. As of December 31, 2021, $2.3 million (before South Korean withholding tax) of development and regulatory milestones have been received under the CKDP Agreement.
94
Additionally, Vifor Pharma Group submitted the payment reimbursement application for TDAPA and HCPCS to CMS in September 2021. In December 2021, CMS granted TDAPA to KORSUVA injection in the anti-pruritic functional category. TDAPA will apply to KORSUVA injection beginning April 1, 2022 for two years. CMS expressed in its written communication to us and Vifor Pharma, a continuing interest in engaging with the companies regarding potential post-TDAPA support to ensure all beneficiaries with ESRD have access to innovative products such as KORSUVA injection. We and Vifor began commercializing KORSUVA injection in the U.S. in December 2021 and we expect commercial launch of KORSUVA injection in April 2022 and associated revenues in the second quarter of 2022.
Our ability to earn these payments and their timing is dependent upon the outcome of I.V. and oral difelikefalin development activities and successful commercialization of KORSUVA injection. However, our receipt of any further such amounts is uncertain at this time and we may never receive any more of these amounts.
Outlook
Based on timing expectations and projected costs for our current clinical development plans, which include conducting supportive Phase 1 trials, Phase 2 trials, and Phase 3 trials of Oral KORSUVA (difelikefalin) in patients with pruritus associated with CKD, CLD, AD, and NP, we expect that our existing cash and cash equivalents and available-for-sale marketable securities as of December 31, 2021 will be sufficient for us to fund our currently anticipated operating expenses and capital requirements through 2023, without giving effect to any potential milestone payments or potential product revenue we may receive under our collaboration agreements with Vifor, VFMCRP, Maruishi and CKDP. Our anticipated operating expenses include contractually committed costs as well as non-contractually committed clinical trial costs for trials that may be delayed or not initiated and other non-committed controllable costs. Because the process of testing product candidates in clinical trials is costly and the timing of progress in these trials is uncertain, it is possible that the assumptions upon which we have based this estimate may prove to be wrong, and we could use our capital resources sooner than we presently expect.
The CARES Act of 2020 and Consolidated Appropriations Act of 2021
On March 27, 2020, President Trump signed into law the CARES Act (H.R. 748), which was further expanded with the signing of the Consolidation Appropriations Act of 2021 (H.R. 133) on December 27, 2020. The CARES Act (and December expansion) includes a variety of economic and tax relief measures intended to stimulate the economy, including loans for small businesses, payroll tax credits/deferrals, and corporate income tax relief. Due to our history of tax loss carryforwards and full valuation allowance, the CARES Act did not have a significant effect to the income tax provision for the years ended December 31, 2021 and 2020, as the corporate income tax relief was directed towards cash taxpayers.
Cash Flows
The following is a summary of the net cash flows provided by (used in) our operating, investing and financing activities for the years ended December 31, 2021, 2020 and 2019:
Year Ended December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
Dollar amounts in thousands | |||||||||
Net cash used in operating activities | $ | (60,087) | $ | (5,487) | $ | (109,225) | |||
Net cash used in investing activities |
| (4,751) |
| (20,275) |
| (30,516) | |||
Net cash provided by financing activities |
| 46,608 |
| 39,140 |
| 142,604 | |||
Net (decrease) increase in cash, cash equivalents and restricted cash | $ | (18,230) | $ | 13,378 | $ | 2,863 | |||
Net cash used in operating activities
Net cash used in operating activities for the year ended December 31, 2021 consisted primarily of a net loss of $88.4 million, partially offset by a $23.1 million cash inflow from net non-cash charges and a $5.3 million cash inflow
95
from net changes in operating assets and liabilities. Net non-cash charges primarily consisted of stock-based compensation expense of $20.8 million, which includes incremental expense related to the modification of our former CEO’s equity awards in 2021 of $5.1 million, the amortization expense component of lease expense of $1.3 million relating to our Stamford operating leases, and the amortization of available-for-sale marketable securities, net of $0.9 million. The change in operating assets and liabilities primarily consisted of an decrease in prepaid expenses of $9.6 million, primarily related to an decrease in prepaid clinical costs, partially offset by a $2.6 million increase in inventory, net as a result of FDA approval of KORSUVA injection in August 2021, a cash outflow of $1.6 million relating to operating lease liabilities associated with our lease agreements for our operating facility in Stamford, Connecticut, and a cash outflow of $1.0 million from a decrease in accounts payable and accrued expenses.
Net cash used in operating activities for the year ended December 31, 2020 consisted primarily of a $7.4 million cash outflow from net changes in operating assets and liabilities and a $6.5 million cash outflow from net non-cash charges, partially offset by net income of $8.4 million (which includes $111.6 million of licensing and milestone fees revenue from the Vifor Agreement). Net non-cash charges primarily consisted of a decrease of $22.3 million in deferred revenue associated with our VFMCRP Agreement, partially offset by stock-based compensation expense of $14.8 million and the amortization expense component of lease expense of $0.8 million relating to our Stamford operating leases. The change in operating assets and liabilities primarily consisted of a cash outflow of $3.2 million from an increase in prepaid expenses, primarily related to an increase in prepaid clinical costs, a cash outflow of $2.8 million from a decrease in accounts payable and accrued expenses, and a cash outflow of $1.1 million relating to operating lease liabilities associated with our Stamford operating leases.
Net cash used in operating activities for the year ended December 31, 2019 consisted primarily of a net loss of $106.4 million and a $3.8 million cash outflow from net non-cash charges, partially offset by a $0.9 million cash inflow from net changes in operating assets and liabilities. Net non-cash charges primarily consisted of a decrease of $19.7 million in deferred revenue associated with our VFMCRP Agreement and $1.4 million related to accretion of available-for-sale securities, partially offset by stock-based compensation expense of $12.6 million and a noncash expense of $4.0 million related to the Enteris License Agreement. The change in operating assets and liabilities primarily consisted of a cash inflow of $6.0 million from an increase in accounts payable and accrued expenses, partially offset by a cash outflow of $4.1 million from an increase in prepaid expense, primarily related to an increase in prepaid clinical costs and a cash outflow of $0.9 million from operating lease liability relating to lease payments made for the Stamford Lease as a result of our adoption of ASC 842: Leases.
Net cash used in investing activities
Net cash used in investing activities was $4.8 million for the year ended December 31, 2021, which primarily included cash outflows of $208.8 million for the purchases of available-for-sale marketable securities, partially offset by cash inflows of $194.0 million from maturities and redemptions of available-for-sale marketable securities and proceeds of $10.0 million from the sales of available-for-sale marketable securities.
Net cash used in investing activities was $20.3 million for the year ended December 31, 2020, which primarily included cash outflows of $232.9 million for the purchases of available-for-sale marketable securities, partially offset by cash inflows of $171.4 million from maturities and redemptions of available-for-sale marketable securities and proceeds of $41.6 million from sales of available-for-sale marketable securities.
Net cash used in investing activities was $30.5 million for the year ended December 31, 2019, which primarily included cash outflows of $286.1 million for the purchases of available-for-sale marketable securities, partially offset by $255.6 million from maturities and redemptions of available-for-sale marketable securities.
Net cash provided by financing activities
Net cash provided by financing activities for the year ended December 31, 2021 consisted of proceeds of $45.0 million from the sale of our common stock relating to a milestone payment received in accordance with the Vifor Agreement and $1.6 million received from the exercise of stock options.
96
Net cash provided by financing activities for the year ended December 31, 2020 consisted of proceeds of $38.4 million from the sale of our common stock relating to the Vifor Agreement and $0.7 million received from the exercise of stock options.
Net cash provided by financing activities for the year ended December 31, 2019 consisted of gross proceeds of $145.5 million from our issuance and sale of our common stock in July 2019, partially offset by $9.0 million of underwriting discounts and commissions and offering expenses paid by us during the year ended December 31, 2019, and proceeds of $6.1 million received from the exercise of stock options.
Critical Accounting Estimates
The preparation of our financial statements and related disclosures in conformity with GAAP and our discussion and analysis of financial condition and results of operations require us to make estimates, judgments and assumptions that affect the reported amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenues and expenses during the reporting period. We base our estimates on historical experience and on various other assumptions that we believe to be reasonable under the circumstances at the time such estimates are made. Actual results and outcomes may differ materially from our estimates, judgments, and assumptions. We periodically review our estimates in light of changes in circumstances, facts, and experience. The effects of material revisions in estimates are reflected in the financial statements prospectively from the date of the change in estimate. Note 2 of Notes to Financial Statements, Summary of Significant Accounting Policies, in this Annual Report on Form 10-K describes the significant accounting policies and methods used in the preparation of our financial statements.
We define our critical accounting estimates as those subjective estimates and judgments about matters that are uncertain and are likely to have a material impact on our financial condition and results of operations as well as the specific manner in which we apply GAAP.
Revenue Recognition
In October 2020, we entered into a royalty-free license agreement with Vifor. Under the Vifor Agreement, we granted Vifor an exclusive license solely in the United States to use, distribute, offer for sale, promote, sell and otherwise commercialize KORSUVA (difelikefalin) injection for all therapeutic uses relating to the inhibition, prevention or treatment of itch associated with pruritus in hemodialysis and peritoneal dialysis patients in the United States. Under the Vifor Agreement, we retain all rights with respect to the clinical development of, and activities to gain regulatory approvals of, KORSUVA (difelikefalin) injection in the United States.
Under the terms of the Vifor Agreement in 2020, we received from Vifor an upfront payment of $100.0 million and an additional payment of $50.0 million for the purchase of an aggregate of 2,939,552 shares of our common stock at a price of $17.0094 per share, which represents a premium over a pre-determined average closing price of our common stock. The purchase of our common stock was governed by the Vifor Stock Purchase Agreement. The excess of the stock purchase price over the cost of the Vifor shares at the closing price of our common stock on the purchase date of $11.6 million was added to the upfront payment and included as license and milestone fees revenue for accounting purposes for the year ended December 31, 2020.
Under the terms of the Vifor Agreement in 2021, we were eligible to receive a non-refundable milestone payment of $50.0 million as consideration for an additional purchase of our common stock upon the regulatory approval by the FDA of KORSUVA injection.
After U.S. regulatory approval of KORSUVA injection by the FDA on August 23, 2021, we received the additional $50.0 million in October 2021 for the purchase of an aggregate of 3,282,391 shares of our common stock at a price of $15.23 per share, which represents a 20% premium to the 30-day trailing average price of our common stock. The purchase of our common stock was governed by the Vifor Stock Purchase Agreement. The excess of the stock purchase price over the cost of the purchased shares at the closing price of our common stock on the date of the
97
achievement of the milestone of $5.0 million was included as license and milestone fees revenue for accounting purposes for the year ended December 31, 2021.
We determined that this critical accounting estimate is subject to uncertainty in 2021 due to the following:
| ● | appropriate measurement of the revenue to be recognized; |
| ● | whether the contract to purchase the shares related to the milestone was a free-standing financial instrument requiring separate accounting; |
| ● | whether a derivative existed; |
| ● | the timing of revenue recognition; and |
| ● | the calculation of the premium paid for the stock recorded as revenue. |
Accounting Pronouncements Recently Adopted; Recent Accounting Pronouncements Not Yet Adopted
We do not expect that any recently issued accounting pronouncements will have a material effect on our financial statements. Refer to Note 2 of Notes to Financial Statements, Summary of Significant Accounting Policies, in this Annual Report on Form 10-K, for a full description of accounting pronouncements recently adopted, and issued but not yet adopted.
Item 7A. Quantitative and Qualitative Disclosures About Market Risk.
Interest Rate Risk
We invest substantially all of our cash reserves in a variety of available-for-sale marketable securities, including investment-grade debt instruments, principally corporate bonds, commercial paper, municipal bonds and direct obligations of the U.S. government and U.S. government-sponsored entities, and in cash equivalents. See Note 3 of Notes to Financial Statements, Available-for-Sale Marketable Securities, in this Annual Report on Form 10-K for details about our available-for-sale marketable securities.
As of December 31, 2021, we had invested $223.3 million of our cash reserves in such marketable securities. Those marketable securities include $223.3 million of investment grade debt instruments with a yield of approximately 0.28% and maturities through November 2024. As of December 31, 2020, we had invested $219.8 million of our cash reserves in such marketable securities. Those marketable securities include $219.8 million of investment grade debt instruments with a yield of approximately 0.32% and maturities through December 2023.
We maintain an investment portfolio in accordance with our investment policy, which includes guidelines on acceptable investment securities, minimum credit quality, maturity parameters, and concentration and diversification. The primary objectives of our investment policy are to preserve principal, maintain proper liquidity and to meet operating needs. Our investments are subject to interest rate risk and will decrease in value if market interest rates increase. However, due to the conservative nature of our investments and relatively short duration, we do not believe we are materially exposed to changes in interest rates related to our investments. As a result, we do not currently use interest rate derivative instruments to manage exposure to interest rate changes.
Duration is a sensitivity measure that can be used to approximate the change in the fair value of a security that will result from a change in interest rates. Applying the duration model, a hypothetical 100 basis point, or 1%, increase in interest rates as of December 31, 2021 and 2020, would have resulted in immaterial decreases in the fair values of our portfolio of marketable securities at those dates.
98
Credit Quality Risk
Although our investments are subject to credit risk, our investment policy specifies credit quality standards for our investments and limits the amount of credit exposure from any single issue, issuer or type of investment. Nonetheless, deterioration of the credit quality of an investment security subsequent to purchase may subject us to the risk of not being able to recover the full principal value of the security. For the years end December 31, 2021 and 2020, we did not record any charges to credit loss expense for our available-for-sale securities. Refer to Note 2 of Notes to Financial Statements, Summary of Significant Accounting Policies – Marketable Securities, in this Annual Report on Form 10-K.
As of December 31, 2021 and 2020, we did not have material balances of receivables on our Balance Sheets.
99
Item 8. Financial Statements and Supplementary Data.
Cara Therapeutics, Inc.
INDEX TO FINANCIAL STATEMENTS
PAGE | |
Reports of Independent Registered Public Accounting Firm (PCAOB ID: | 101 |
Financial Statements: | |
104 | |
105 | |
106 | |
107 | |
108 |
100
Report of Independent Registered Public Accounting Firm
To the Shareholders and the Board of Directors of Cara Therapeutics, Inc.
Opinion on the Financial Statements
We have audited the accompanying balance sheets of Cara Therapeutics, Inc. (the Company) as of December 31, 2021 and 2020, the related statements of comprehensive (loss) income, stockholders' equity and cash flows for each of the three years in the period ended December 31, 2021, and the related notes (collectively referred to as the “financial statements”). In our opinion, the financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2021 and 2020, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2021, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company's internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) and our report dated March 1, 2022 expressed an unqualified opinion thereon.
Basis for Opinion
These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matter
The critical audit matter communicated below is a matter arising from the current period audit of the financial statements that was communicated or required to be communicated to the audit committee and that: (1) relates to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective or complex judgments. The communication of the critical audit matter does not alter in any way our opinion on the financial statements, taken as a whole, and we are not, by communicating the critical audit matter below, providing a separate opinion on the critical audit matter or on the account or disclosure to which it relates.
Revenue Recognition | ||
Description of the Matter | As discussed in Notes 12 and 13 to the financial statements, the Company entered into a royalty-free license agreement and corresponding securities purchase agreement with Vifor (International) Ltd. (“Vifor”) on October 15, 2020, whereby the Company granted Vifor exclusive commercialization rights to its product candidates in the United States. Pursuant to these agreements, the Company was eligible to receive a non-refundable milestone payment of $50 million as consideration for an additional purchase of the Company’s common stock upon the first regulatory approval by the FDA of the Licensed Product for the Pruritus CKD - Hemodialysis indication, which occurred on August 23, 2021. Upon FDA approval and satisfaction of the contingency, to determine the measurement of the revenue to be recognized during the period, the |
101
Company assessed whether the contract to purchase the shares related to the milestone was a free standing financial instrument requiring separate accounting, whether a derivative existed, the timing of revenue recognition and the calculation of the premium paid for the stock recorded as revenue. Auditing revenue recognition is complex and involves a degree of subjective auditor judgment to determine if revenue should be recognized and the related timing and amount of revenue recognized. | ||
How We Addressed the Matter in Our Audit | We obtained an understanding, evaluated the design, and tested the operating effectiveness of controls relating to the revenue recognition process, including controls over management’s review of the terms and conditions of the license and securities purchase agreements, evaluation of the accounting related to the achievement of the milestone and the measurement of the premium paid for common stock recorded as revenue for the period.
To test the amount of revenue recognized, we, among other things, assessed the Company’s evaluation of the accounting related to the license and securities agreements, verified the milestone was achieved and tested the measurement of the premium paid for the stock which was recognized as revenue during the period. |
/s/
We have served as the Company's auditor since 2006.
March 1, 2022
102
Report of Independent Registered Public Accounting Firm
To the Shareholders and the Board of Directors of Cara Therapeutics, Inc.
Opinion on Internal Control Over Financial Reporting
We have audited Cara Therapeutics, Inc.’s internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the COSO criteria). In our opinion, Cara Therapeutics, Inc. (the Company) maintained, in all material respects, effective internal control over financial reporting as of December 31, 2021, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the balance sheets of the Company as of December 31, 2021 and 2020, the related statements of comprehensive (loss) income, stockholders' equity and cash flows for each of the three years in the period ended December 31, 2021, and the related notes and our report dated March 1, 2022 expressed an unqualified opinion thereon.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects.
Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control Over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ Ernst & Young LLP
Stamford, Connecticut
March 1, 2022
103
CARA THERAPEUTICS, INC.
BALANCE SHEETS
(amounts in thousands, except share and per share data)
| December 31, 2021 |
| December 31, 2020 | |||
Assets |
|
|
| |||
Current assets: |
|
|
|
| ||
Cash and cash equivalents | $ | | $ | | ||
Marketable securities |
| |
| | ||
Income tax receivable |
| |
| | ||
Other receivables |
| |
| | ||
Inventory, net | | — | ||||
Prepaid expenses |
| |
| | ||
Total current assets |
| |
| | ||
Operating lease right-of-use assets | | | ||||
Marketable securities, non-current |
| |
| | ||
Property and equipment, net |
| |
| | ||
Restricted cash |
| |
| | ||
Total assets | $ | | $ | | ||
Liabilities and stockholders’ equity |
|
|
| |||
Current liabilities: |
|
|
|
| ||
Accounts payable and accrued expenses | $ | | $ | | ||
Operating lease liabilities, current |
| |
| | ||
Total current liabilities |
| |
| | ||
Operating lease liabilities, non-current | | | ||||
Commitments and contingencies (Note 18) |
|
| ||||
Stockholders’ equity: |
|
|
|
| ||
Preferred stock; $ |
|
| ||||
Common stock; $ |
| |
| | ||
Additional paid-in capital |
| |
| | ||
Accumulated deficit |
| ( |
| ( | ||
Accumulated other comprehensive (loss) income |
| ( |
| | ||
Total stockholders’ equity |
| |
| | ||
Total liabilities and stockholders’ equity | $ | | $ | | ||
See Notes to Financial Statements.
104
CARA THERAPEUTICS, INC.
STATEMENTS OF COMPREHENSIVE (LOSS) INCOME
(amounts in thousands, except share and per share data)
Year Ended December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
Revenue: | |||||||||
License and milestone fees | $ | | $ | | $ | | |||
Collaborative revenue |
| |
| — |
| — | |||
Commercial supply revenue | | — | — | ||||||
Clinical compound revenue |
| |
| |
| | |||
Total revenue |
| |
| |
| | |||
Operating expenses: |
|
|
|
|
|
| |||
Research and development |
| |
| |
| | |||
General and administrative |
| |
| |
| | |||
Total operating expenses |
| |
| |
| | |||
Operating (loss) income |
| ( |
| |
| ( | |||
Other income, net |
| |
| |
| | |||
(Loss) income before income tax benefit |
| ( |
| |
| ( | |||
Income tax benefit |
| — |
| |
| | |||
Net (loss) income | $ | ( | $ | | $ | ( | |||
Net (loss) income per share: |
|
|
|
|
|
| |||
Basic | $ | ( | $ | | $ | ( | |||
Diluted | $ | ( | $ | | $ | ( | |||
Weighted average shares: |
|
|
|
|
| ||||
Basic |
| |
| |
| | |||
Diluted | | | | ||||||
Other comprehensive (loss) income, net of tax of $ |
|
|
|
|
|
| |||
Change in unrealized (losses) gains on available-for-sale marketable securities |
| ( |
| ( |
| | |||
Total comprehensive (loss) income | $ | ( | $ | | $ | ( | |||
See Notes to Financial Statements.
105
CARA THERAPEUTICS, INC.
STATEMENTS OF STOCKHOLDERS’ EQUITY
(amounts in thousands, except share and per share data)
Accumulated | |||||||||||||||||
Additional | Other | Total | |||||||||||||||
Common Stock | Paid-In | Accumulated | Comprehensive | Stockholders’ | |||||||||||||
| Shares |
| Amount |
| Capital |
| Deficit |
| (Loss) Income |
| Equity | ||||||
Balance at December 31, 2018 | | $ | | $ | | $ | ( | $ | ( | $ | | ||||||
Sale of common stock in a follow-on public offering ($ |
| |
| |
| |
| — |
| — |
| | |||||
Issuance of common stock upon entry into License Agreement with Enteris Biopharma, Inc. ($ |
| |
| — |
| |
| — |
| — |
| | |||||
Stock-based compensation expense | — | — | | — | — | | |||||||||||
Shares issued upon exercise of stock options | | | | — | — | | |||||||||||
Shares issued upon vesting of restricted stock units | | — | | — | — | | |||||||||||
Shares issued for consulting services | | — | | — | — | | |||||||||||
Net loss |
| — |
| — |
| — |
| ( |
| — |
| ( | |||||
Other comprehensive income |
| — |
| — |
| — |
| — |
| |
| | |||||
Balance at December 31, 2019 | | $ | | $ | | $ | ( | $ | | $ | | ||||||
Sale of common stock under license agreement with Vifor ($ | | | | — | — | | |||||||||||
Stock-based compensation expense | — |
| — |
| |
| — |
| — |
| | ||||||
Shares issued upon exercise of stock options | |
| — |
| |
| — |
| — |
| | ||||||
Shares issued upon vesting of restricted stock units | |
| — |
| |
| — |
| — |
| | ||||||
Net income | — |
| — |
| — |
| |
| — |
| | ||||||
Other comprehensive loss | — |
| — |
| — |
| — |
| ( |
| ( | ||||||
Balance at December 31, 2020 | | $ | | $ | | $ | ( | $ | | $ | | ||||||
Sale of common stock under license agreement with Vifor ($ | | | | — | — | | |||||||||||
Stock-based compensation expense | — | — | | — | — | | |||||||||||
Shares issued upon exercise of stock options | | — | | — | — | | |||||||||||
Shares issued upon vesting of restricted stock units | | — | | — | — | | |||||||||||
Net loss | — | — | — | ( | — | ( | |||||||||||
Other comprehensive loss | — | — | — | — | ( | ( | |||||||||||
Balance at December 31, 2021 | | $ | | $ | | $ | ( | $ | ( | $ | | ||||||
See Notes to Financial Statements.
106
CARA THERAPEUTICS, INC.
STATEMENTS OF CASH FLOWS
(in thousands)
Year Ended December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
Operating activities |
|
|
|
| |||||
Net (loss) income | $ | ( | $ | | $ | ( | |||
Adjustments to reconcile net (loss) income to net cash used in operating activities: |
|
|
|
|
|
| |||
Stock-based compensation expense |
| |
| |
| | |||
Depreciation and amortization |
| |
| |
| | |||
Amortization expense component of lease expense |
| |
| |
| | |||
Noncash expense related to oral formulation license agreement | — | — | | ||||||
Amortization (accretion) of available-for-sale marketable securities, net | | | ( | ||||||
Realized gain on sale of available-for-sale marketable securities |
| ( |
| ( |
| — | |||
Realized gain on sale of property and equipment |
| ( |
| — |
| — | |||
Deferred revenue |
| — |
| ( |
| ( | |||
Changes in operating assets and liabilities: |
|
|
|
| |||||
Income tax receivable | | ( | ( | ||||||
Other receivables |
| |
| |
| ( | |||
Inventory, net | ( | — | — | ||||||
Prepaid expenses |
| |
| ( |
| ( | |||
Accounts payable and accrued expenses |
| ( |
| ( |
| | |||
Operating lease liabilities | ( | ( | ( | ||||||
Net cash used in operating activities |
| ( |
| ( |
| ( | |||
Investing activities |
|
|
|
|
|
| |||
Proceeds from maturities of available-for-sale marketable securities |
| |
| |
| | |||
Proceeds from redemptions of available-for-sale marketable securities, at par | | | | ||||||
Proceeds from sale of available-for-sale marketable securities |
| |
| |
| — | |||
Purchases of available-for-sale marketable securities |
| ( |
| ( |
| ( | |||
Proceeds from sale of property and equipment |
| |
| — |
| — | |||
Purchases of property and equipment | ( | ( | ( | ||||||
Net cash used in investing activities |
| ( |
| ( |
| ( | |||
Financing activities |
|
|
|
|
| ||||
Proceeds from the sale of common stock under license agreement with Vifor |
| |
| |
| — | |||
Proceeds from the sale of common stock in a follow-on public offering, net of issuance costs |
| — |
| — |
| | |||
Proceeds from the exercise of stock options |
| |
| |
| | |||
Net cash provided by financing activities |
| |
| |
| | |||
Net (decrease) increase in cash, cash equivalents and restricted cash |
| ( |
| |
| | |||
Cash, cash equivalents and restricted cash at beginning of period |
| |
| |
| | |||
Cash, cash equivalents and restricted cash at end of period | $ | | $ | | $ | | |||
Noncash investing and financing activities |
|
| |||||||
Shares of common stock issued in connection with oral formulation license agreement | $ | — | $ | — | $ | | |||
Shares of common stock issued in exchange for consulting services | $ | — | $ | — | $ | | |||
See Notes to Financial Statements.
107
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
1. Business
Cara Therapeutics, Inc., or the Company, is an early commercial-stage biopharmaceutical corporation formed on
On August 23, 2021, the Company received U.S. Food and Drug Administration, or FDA, approval for KORSUVATM (difelikefalin) injection, or KORSUVA injection, for the treatment of moderate-to-severe pruritus associated with chronic kidney disease in adults undergoing hemodialysis. The Company has a license agreement with Vifor (International) Ltd., or Vifor, that provides full commercialization rights of KORSUVA injection to Vifor in dialysis clinics in the United States under a profit-sharing arrangement, whereby total net sales of KORSUVA injection in the U.S., as recorded by Vifor, are reduced by a marketing and distribution fee owed by the Company based on the level of annual net sales, and the resulting amount is shared according to a
As of December 31, 2021, the Company has raised aggregate net proceeds of approximately $
As of December 31, 2021, the Company had unrestricted cash and cash equivalents and marketable securities of $
The Company is subject to risks common to other life science companies including, but not limited to, uncertainty of product development and commercialization, lack of marketing and sales history, development by its competitors of new technological innovations, dependence on key personnel, market acceptance of products, product liability, protection of proprietary technology, ability to raise additional financing, and compliance with the FDA and other government regulations. If the Company does not successfully commercialize KORSUVA injection or any of its other product candidates, it will be unable to generate additional recurring product revenue or achieve profitability.
108
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
2. Summary of Significant Accounting Policies
Use of Estimates
The preparation of financial statements in conformity with generally-accepted accounting principles in the United States, or GAAP, requires the Company to make estimates and assumptions that affect the reported amounts of assets and liabilities, and disclosure of contingent assets and liabilities, as of the date of the financial statements as well as the reported amounts of revenues and expenses during the reporting period. The more significant estimates include the fair value of marketable securities that are classified as level 2 of the fair value hierarchy, the amount and periods over which certain revenues will be recognized, including licensing and collaborative revenue recognized from non-refundable up-front and milestone payments, related party accounts receivable, inventory valuation and related reserves, the determination of prepaid research and development, or R&D, clinical costs and accrued research projects, the amount of non-cash compensation costs related to share-based payments to employees and non-employees, the incremental borrowing rate used in lease calculations and the likelihood of realization of deferred tax assets.
The ongoing COVID-19 pandemic has interrupted business operations across the globe. Estimates and assumptions about future events and their effects cannot be determined with certainty and therefore require the exercise of judgment. As of the date of issuance of these financial statements, the Company is not aware of any specific event or circumstance that would require the Company to update its estimates, assumptions and judgments or revise the reported amounts of assets and liabilities or the disclosure of contingent assets and liabilities. These estimates, however, may change as new events occur and additional information is obtained, and are recognized in the financial statements as soon as they become known.
Actual results could differ materially from the Company’s estimates and assumptions.
Concentration of Credit Risk
Financial instruments, which potentially subject the Company to significant concentrations of credit risk consist primarily of cash and cash equivalents, marketable securities, and related party accounts receivable. The Company invests its cash reserves in money market funds or high-quality marketable securities in accordance with its investment policy. The stated objectives of its investment policy are to preserve capital, provide liquidity consistent with forecasted cash flow requirements, maintain appropriate diversification and generate returns relative to these investment objectives and prevailing market conditions. The Company’s investment policy includes guidelines on acceptable investment securities, limits interest-bearing security investments to certain types of debt and money market instruments issued by the U.S. government and institutions with investment grade credit ratings and places restrictions on maturities and concentration by asset class and issuer. The Company’s cash and cash equivalents and marketable securities are held by
109
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
The percentages of revenue recognized from license agreement partners of the Company in the years ended December 31, 2021, 2020 and 2019 are included in the following table:
Revenue |
| ||||||
Year Ended December 31, |
| ||||||
| 2021 |
| 2020 |
| 2019 |
| |
License Agreement Partner: |
|
|
|
|
|
| |
VFMCRP |
| | % | | % | | % |
Vifor |
| | % | | % | — | % |
For the years ended December 31, 2021, 2020 and 2019, no additional license agreement partners or customers accounted for more than 10% of the Company’s revenue.
Concentration of Suppliers
The Company relies on
Cash and Cash Equivalents
Cash and cash equivalents include cash on hand, demand deposits, deposits with banks and highly liquid money market funds with holdings of cash and other investments with original maturities of three months or less.
Marketable Securities
On January 1, 2020, the Company adopted Accounting Standards Update, or ASU, No. 2016-13, Financial Instruments—Credit Losses (Topic 326), Measurement of Credit Losses on Financial Instruments, or ASU 2016-13, which replaced the incurred loss impairment methodology in prior GAAP that delayed recognition of a credit loss until it is probable that such loss has been incurred, with a methodology that reflects expected credit losses and requires consideration of a broader range of reasonable and supportable information to inform credit loss estimates.
The Company deems certain of its investments to be marketable securities if the investment, or in the case of money market funds, the securities underlying the money market fund, meet the definition of a debt security in Accounting Standards Codification, or ASC, section 320-10-20. The Company considers its marketable securities to be available-for-sale, which are its only financial instruments that are within the scope of ASU 2016-13 as of December 31, 2021. The Company’s investments in marketable securities, including U.S. Treasury securities, U.S. government agency obligations, corporate bonds, commercial paper, and municipal bonds are highly rated by Moody’s and S&P and have maturities primarily of less than one year but no longer than three years. Accordingly, credit risk associated with the Company’s available-for-sale debt security portfolio is mitigated.
ASU 2016-13 modifies the prior other-than-temporary impairment model for available-for-sale debt securities by requiring (1) estimating expected credit losses (the portion of the amortized cost basis of a financial asset that the Company does not expect to collect) only when the fair value is below the amortized cost of the asset; (2) recording a credit loss without regard to the length of time a security has been in an unrealized loss position; (3) limiting the measurement of the credit loss to the difference between the security’s amortized cost basis and its fair value; and
110
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
(4) presenting credit losses as an allowance rather than as a write-down, which will allow the Company to record reversals of credit losses in current period net income, a practice that was previously prohibited.
The Company reviews each of its available-for-sale marketable securities for unrealized losses (declines in fair value below its amortized cost basis) at each balance sheet date presented in its financial statements and whenever events or changes in circumstances indicate that the amortized cost basis of an asset may not be recoverable. In accordance with the adoption of ASU 2016-13, the Company is required to determine whether any portion of the unrealized loss for any available-for-sale debt security is due to a credit loss, and if so, to measure the amount of the credit loss.
The Company will rely on both qualitative and quantitative factors to determine whether the unrealized loss for each available-for-sale debt security at any balance sheet date is due to a credit loss.
Qualitative factors may include a credit downgrade, severity of the decline in fair value below amortized cost and other adverse conditions related specifically to the security, as well as the intent to sell the security, or whether the Company will more likely than not be required to sell the security before recovery of its amortized cost basis. The Company’s assessment of whether a security is impaired could change in the future due to new developments or changes in assumptions related to any particular security. If material qualitative factors indicate that a credit loss has occurred, the Company will determine the magnitude of that credit loss using a discounted cash flow model or other quantitative method.
If the Company intends to sell the security or it is more likely than not that the Company will be forced to sell the security before recovery of the amortized cost of the security, the entire unrealized loss is deemed to be a credit loss, which is recognized in net (loss) income. Otherwise, the portion of the unrealized loss that is due to a credit loss will be recorded as an allowance for credit loss, which will offset the balance of marketable securities and as credit loss expense within other income, net. The portion of the unrealized loss that is not due to a credit loss as well as all unrealized gains will be recorded in Accumulated Other Comprehensive Income (Loss). There was no cumulative effect adjustment as a result of the adoption of ASU 2016-13 on January 1, 2020 (see Note 3, Available-for-Sale Marketable Securities, and Note 11, Fair Value Measurements).
Accrued interest receivables are excluded from the Company’s amortized cost bases for its available-for-sale marketable securities and are included within Other receivables. The Company’s policy is to not measure an allowance for credit losses on accrued interest receivable balances at each reporting period since it elects to write off uncollectible accrued interest receivable balances as credit loss expense in a timely manner, which is by maturity date for all categories of its debt securities.
Fair Value of Financial Instruments
The Company applies fair value accounting for all financial assets and liabilities that are recognized or disclosed at fair value in the financial statements on a recurring basis. The Company defines fair value as the price that would be received from selling an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date. When determining the fair value measurements for assets and liabilities which are required to be recorded at fair value, the Company considers the principal or most advantageous market in which it would transact and the market-based risk measurements or assumptions that market participants would use in pricing the asset or liability, such as risks inherent in valuation techniques, transfer restrictions and credit risks.
The Company’s financial instruments consist of cash, cash equivalents, available-for-sale marketable securities, prepaid expenses, restricted cash, accounts payable and accrued liabilities. The fair values of cash, cash equivalents, prepaid expenses, restricted cash, accounts payable and accrued liabilities approximate their carrying values due to the short-term nature of these financial instruments. Available-for-sale marketable securities are reported as marketable
111
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
securities at their fair values, based upon pricing of securities with the same or similar investment characteristics as provided by third-party pricing services, as described below.
The valuation techniques used by the Company are based on observable and unobservable inputs. Observable inputs reflect readily obtainable data from independent sources, while unobservable inputs reflect the Company’s assumptions about the inputs that market participants would use in pricing the asset or liability and are developed based on the best information available in the circumstances.
The Company classifies its investments in a fair value hierarchy that is intended to increase consistency and comparability in fair value measurements and related disclosures. The fair value hierarchy is divided into three levels based on the source of inputs as follows:
| ● | Level 1 – Observable inputs – quoted prices in active markets for identical assets and liabilities. |
| ● | Level 2 – Observable inputs other than the quoted prices in active markets for identical assets and liabilities – such as quoted prices for similar instruments, quoted prices for identical or similar instruments in inactive markets, or other inputs that are observable or can be corroborated by observable market data. |
| ● | Level 3 – Unobservable inputs – includes amounts derived from valuation models where one or more significant inputs are unobservable and require the Company to develop relevant assumptions. |
The Company records transfers between levels in the hierarchy by assuming that the transfer occurred at the end of the quarter or year-to-date period.
Valuation Techniques - Level 2 Inputs
The Company estimates the fair values of its financial instruments categorized as level 2 in the fair value hierarchy, including U.S. Treasury securities, U.S. government agency obligations, corporate bonds, commercial paper and municipal bonds, by taking into consideration valuations obtained from third-party pricing services. The pricing services use industry standard valuation models, including both income- and market-based approaches, for which all significant inputs are observable, either directly or indirectly, to estimate fair value. These inputs include reported trades of and broker/dealer quotes on the same or similar securities, benchmark yields, issuer credit spreads, benchmark securities, and other observable inputs. The Company obtains a single price for each financial instrument and does not adjust the prices obtained from the pricing service.
The Company validates the prices provided by its third-party pricing services by reviewing their pricing methods, obtaining market values from other pricing sources and comparing them to the share prices presented by the third-party pricing services. After completing its validation procedures, the Company did not adjust or override any fair value measurements provided by its pricing services as of December 31, 2021 or December 31, 2020.
Inventory, net
Inventories are stated at the lower of cost or net realizable value. The Company determines the cost of inventory using first-in, first-out, or FIFO, method.
The Company capitalizes inventory costs associated with the Company’s products prior to regulatory approval, when, based on management’s judgment, future commercialization is considered probable and the future economic benefit is expected to be realized; otherwise, such costs are expensed. The determination to capitalize inventory costs is based on various factors, including status and expectations of the regulatory approval process, any known safety or
112
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
efficacy concerns, potential labeling restrictions, and any other impediments to obtaining regulatory approval. As KORSUVA injection is the Company’s first commercial product and probability could not be established prior to regulatory approval on August 23, 2021, all inventory costs prior to regulatory approval were expensed as incurred.
The Company periodically analyzes its inventory levels to identify inventory that may expire prior to expected sale or has a cost basis in excess of its estimated realizable value and writes down such inventories as appropriate. In addition, the Company’s products are subject to strict quality control and monitoring which the Company performs throughout the manufacturing process. If certain batches or units of product no longer meet quality specifications or become obsolete due to expiration, the Company records a charge to write down such unmarketable inventory to its estimated realizable value.
Property and Equipment, net
Property and equipment (consisting of computer and office equipment, furniture and fixtures and leasehold improvements) are stated at cost, net of accumulated depreciation and amortization of leasehold improvements. Depreciation and amortization are calculated using the straight-line method over the estimated useful lives of the respective assets. Leasehold improvements are amortized over the lesser of their useful lives or the life of the lease.
Asset Category |
| Useful Lives |
Computer and office equipment |
| |
Furniture and fixtures |
| |
Leasehold improvements |
|
The Company reviews the recorded values of property and equipment for impairment whenever events or changes in business circumstances indicate that the carrying amount of an asset or group of assets may not be fully recoverable.
Revenue Recognition
Under ASU 2014-09, Revenue from Contracts with Customers (Topic 606), or ASC 606, as amended by ASU 2016-08, 2016-10, 2016-12 and 2016-20, the Company recognizes revenue in an amount that reflects the consideration to which it expects to be entitled in exchange for the transfer of promised goods or services to customers. To determine revenue recognition for contracts with customers that are within the scope of ASC 606, the Company performs the following steps: (1) identifies the contract with the customer, (2) identifies the performance obligations in the contract, (3) determines the transaction price, (4) allocates the transaction price to the performance obligations in the contract, and (5) recognizes revenue when (or as) the entity satisfies a performance obligation.
The Company has entered into agreements to license its intellectual property, or IP, related to difelikefalin to develop, manufacture and/or commercialize drug products. These agreements typically contain multiple performance obligations, including licenses of IP and R&D services. Payments to the Company under these agreements may include nonrefundable license fees, payments for research activities, payments based upon the achievement of certain milestones and royalties on any resulting net product sales. The Company receives its share of the net profits from the sale of KORSUVA injection in the U.S. through its license agreement with Vifor. The Company has adopted a policy to recognize revenue net of tax withholdings, as applicable.
The Company identifies agreements as contracts that create enforceable rights and obligations when the agreement is approved by the parties, identifies the rights of the parties and the payment terms, has commercial substance and it is probable that the Company will collect the consideration to which it will be entitled in exchange for the goods and services that will be transferred to the customer. The counterparty is considered to be a customer when it has contracted
113
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
with the Company to obtain goods and services that are the output of the Company’s ordinary activities (i.e., development of pharmaceutical products) in exchange for consideration.
A performance obligation is a promise to transfer distinct goods or services to a customer. Performance obligations that are both capable of being distinct and distinct within the context of the contract are considered to be separate performance obligations. Performance obligations are capable of being distinct if the counterparty is able to benefit from the good or service on its own or together with other resources that are readily available to it. Performance obligations are distinct within the context of the contract when each performance obligation is separately identifiable from each other; i.e., the Company is not using the goods or services as inputs to produce or deliver the combined output or outputs specified by the customer; one or more of the goods or services does not significantly modify or customize one of the other goods or services in the contract; and goods or services are not highly interdependent or not highly interrelated. Performance obligations that are not distinct are accounted for as a single performance obligation over the period that goods or services are transferred to the customer. The determination of whether performance obligations in a contract are distinct may require significant judgment.
The transaction price is the amount of consideration that the Company expects to be entitled to in exchange for transferring promised goods or services to the customer based on the contract terms at inception of a contract. There is a constraint on inclusion of variable consideration related to licenses of IP, such as milestone payments or sales-based royalty payments, in the transaction price if there is uncertainty at inception of the contract as to whether such consideration will be recognized in the future because it is probable that there will be a significant reversal of revenue in the future when the uncertainty is resolved. The determination of whether or not it is probable that a significant reversal of revenue will occur in the future depends on the likelihood and magnitude of the reversal. Factors that could increase the likelihood or magnitude of a reversal of revenue include (a) the susceptibility of the amount of consideration to factors outside the entity’s influence, such as the outcome of clinical trials, the timing of initiation of clinical trials by the counterparty and the approval of drug product candidates by regulatory agencies, (b) situations in which the uncertainty is not expected to be resolved for a long period of time, and (c) level of the Company’s experience in the field. When it becomes probable that events will occur, for which variable consideration was constrained at inception of the contract, the Company allocates the related consideration to the separate performance obligations in the same manner as described below.
At inception of a contract, the Company allocates the transaction price to the distinct performance obligations based upon their relative standalone selling prices. Standalone selling price is the price at which an entity would sell a promised good or service separately to a customer. The best evidence of standalone selling price is an observable price of a good or service when sold separately by an entity in similar circumstances to similar customers. Since the Company typically does not have such evidence, it estimates standalone selling price so that the amount that is allocated to each performance obligation equals the amount that the Company expects to receive for transferring goods or services. The methods that the Company uses to make such estimates include (1) the adjusted market assessment approach, under which the Company forecasts and analyzes difelikefalin in the appropriate market, the phase of clinical development as well as considering recent similar license arrangements within the same phase of clinical development, therapeutic area, type of agreement, etc. and (2) the expected cost of satisfying the performance obligations plus a margin, or the expected cost plus a margin approach.
The Company recognizes revenue when, or as, it satisfies a performance obligation by transferring a promised good or service to a customer and the customer obtains control of the good or service. Revenue related to the grant of a license that is a distinct performance obligation and that is deemed to be functional IP is recognized at the point in time that the Company has the right to payment for the license, the customer has legal title to the license and can direct the use of the license (for example, to grant sublicenses), the customer has the significant risks and rewards of ownership of the license and the customer has accepted the asset (license) by signing the license agreement.
114
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Recognition of revenue related to R&D services that are a distinct performance obligation or that are combined with granting of a license as a single performance obligation is deferred at inception of a contract and is recognized as those services are performed based on the costs incurred as a percentage of the estimated total costs to be incurred to complete the performance obligation.
Milestone payments are considered to be variable consideration and are not included in the transaction price at inception of the contract if it is uncertain that the milestone will be achieved. Rather, when it becomes probable that the milestone will be achieved and, therefore, there will not be a significant reversal of revenue in future periods, the respective amount to be earned is included in the transaction price, allocated to the distinct performance obligations based on their relative standalone selling price and recognized as revenue, as described above. Sales milestones and sales-based royalty payments related to a license of IP are recognized as revenue when the respective sales occur.
License and Milestone Fees
License and milestone fees include upfront and milestone payments associated with the Company’s license agreements with Vifor, VFMCRP, Maruishi and CKDP. All upfront and milestone payments associated with the license agreements with Vifor, VFMCRP and CKDP are recognized as license and milestone fees since they contain only
Collaborative Revenue
Collaborative revenue includes milestone payments associated with the Company’s license agreement with Maruishi that were allocated to the R&D services performance obligation (see Note 13, Revenue Recognition).
Commercial Supply Revenue
Commercial supply revenue includes sales of KORSUVA injection commercial product to Vifor, which ultimately will act as the principal in the net profit-sharing arrangement between the
Clinical Compound Revenue
Clinical compound revenue includes sales of clinical compound to Vifor (prior to FDA approval), VFMCRP, and Maruishi for the years ended December 31, 2021, 2020 and 2019. The Company recognizes revenue on clinical compound sales when control has transferred to Vifor, VFMCRP and Maruishi, which occurs at a point in time, typically upon receipt of the clinical compound, and generally occurs after the clinical compound has passed all quality testing required for acceptance. The sales of clinical compound are reimbursed at COGS plus an agreed upon margin.
Cost of Goods Sold (COGS)
COGS includes costs related to sales of the Company’s commercial product, KORSUVA injection, to Vifor. Costs related to the sales of KORSUVA injection are generally recognized upon receipt of shipment by Vifor. The Company’s COGS for KORSUVA injection includes the cost of producing commercial product that correspond with commercial
115
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
supply revenue, such as third-party supply and overhead costs, as well as certain period costs related to freight, packaging, stability, and quality testing. For the year ended December 31, 2021,
Research and Development (R&D) Expenses
R&D costs are charged to expense as incurred. Costs incurred under agreements with third parties are charged to expense as incurred in accordance with the specific contractual performance terms of such agreements. R&D expenses include, among other costs, compensation and other personnel-related costs, including consultant costs, and costs to conduct clinical trials using clinical research organizations, or CROs, which include upfront, milestone and monthly expenses as well as reimbursement for pass through costs. The amount of clinical trial expense recognized in any period varies depending on the duration and progress of each clinical trial, including the required level of patient enrollment, the rate at which patients actually enroll in and drop-out of the clinical trial, and the number of sites involved in the trial as well as the activities to be performed by the sites each period. R&D costs also include costs to manufacture product candidates and clinical supplies, laboratory supplies costs, facility-related costs and stock-based compensation for R&D personnel. Non-refundable R&D advance payments are deferred and capitalized as prepaid R&D expense. The capitalized amounts are expensed as the related goods are delivered or services are performed. As of December 31, 2021 and 2020, the Company recorded $
General and Administrative (G&A) Expenses
G&A costs are charged to expense as incurred. G&A expenses consist primarily of salaries and other related costs, including stock-based compensation, for personnel in executive, finance, accounting, legal, business development, information technology and human resources functions. Other costs include facility costs not otherwise included in R&D expenses, legal fees, insurance costs, investor relations costs, patent costs and fees for accounting and consulting services.
As noted in Note 12, Collaboration and Licensing Agreements, the Company’s license agreement with Vifor provides full commercialization rights of KORSUVA injection to Vifor under a profit-sharing arrangement. Under this profit-sharing arrangement, in consideration of Vifor’s conduct of the marketing, promotion, selling and distribution of KORSUVA injection in the U.S., the Company will pay a marketing and distribution fee to Vifor based on the level of annual net sales. This fee will be deducted from product sales in calculating the net profits that are subject to the profit-sharing arrangement.
Income Taxes
The Company accounts for income taxes using the asset and liability method. Under this method, deferred tax assets and liabilities are determined based on differences between the financial reporting and tax bases of assets and liabilities and are measured using the enacted tax rates and laws that will be in effect when the differences are expected to reverse. Deferred income tax assets are reduced, as necessary, by a valuation allowance when management determines it is more likely than not that some or all of the tax benefits will not be realized.
There were no material uncertain tax positions taken as of December 31, 2021 and 2020. The Company does not have any interest or penalties accrued related to tax positions as it does not have any unrecognized tax benefits. In the event the Company determines that accrual of interest or penalties are necessary in the future, the amount will be presented as a component of interest expense.
116
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Stock-Based Compensation
The Company grants stock options to employees, non-employee members of the Company’s Board of Directors and non-employee consultants as compensation for services performed. All share-based payments, including grants of stock options, are recognized based on their grant date fair values. The grant date fair value of stock options is estimated using the Black-Scholes option valuation model.
Using this model, fair value is calculated based on assumptions with respect to (i) the fair value or market price of the Company’s common stock on the grant date; (ii) expected volatility of the Company’s common stock price, (iii) the periods of time over which employees and members of the Company’s Board of Directors or non-employee consultants are expected to hold their options prior to exercise (expected term), (iv) expected dividend yield on the Company’s common stock, and (v) risk-free interest rates.
The Company’s common stock has been traded on a public exchange only since January 31, 2014. Since that time, exercises of stock options have been limited due to various factors, including fluctuations in the Company’s stock price to below the exercise prices of awards and blackout periods during which exercises are not allowed, among others. Therefore, the Company believes that as of December 31, 2021, it does not have sufficient company-specific information available to determine the expected term based on its historical data. As a result, the expected term of stock options granted is determined using the average of the vesting period and term (
The Company calculates the expected volatility using company-specific trading activity of its common stock over the option’s expected term.
The expected dividend yield is
The Company’s policy is to account for forfeitures of share-based payments as they occur.
Compensation cost for all share-based payments granted with service-based graded vesting schedules is recognized using the straight-line method over the requisite service period.
(Loss) Income Per Share
The Company computes basic net (loss) income per share by dividing net (loss) income by the weighted average number of shares of common stock outstanding. Diluted net (loss) income per share includes the potential dilutive effect of common stock equivalents as if such securities were converted or exercised during the period, when the effect is dilutive. Common stock equivalents may include outstanding stock options and restricted stock units, which are included under the treasury stock method when dilutive. For each of the years ended December 31, 2021 and 2019, the Company excluded the effects of potentially dilutive shares that were outstanding during those respective periods from the denominator as their inclusion would have been anti-dilutive due to the Company’s net losses for those periods. For the year ended December 31, 2020, the Company included the effects of dilutive shares that were outstanding in the denominator as their inclusion was dilutive due to the Company’s net income for the period.
Segment Reporting
Operating segments are identified as components of an enterprise about which separate discrete financial information is available for evaluation by the chief operating decision-maker in making decisions regarding resource
117
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
allocation and assessing performance. The Company views its operations and manages its business as
Leases
The Company has
In general, the Company determines if a contract, at its inception, is a lease or contains a lease based on whether the contract conveys the right to control the use of identified property, plant, or equipment (an identified asset) for a period of time in exchange for consideration. To determine whether a contract conveys the right to control the use of an identified asset for a period of time, the Company assesses whether, throughout the period of use, it has both the right to obtain substantially all of the economic benefits from use of the identified asset, and the right to direct the use of the identified asset. Both of these criteria are met by the Stamford Lease.
Under ASC 842, the Company determines the amount of the operating lease liability based on the present value of the future minimum lease payments over the remaining lease term. The amount of the operating lease ROU asset is equal to the amount of the lease liability, less accrued rent and lease incentives received from the landlord. Initial direct costs were deemed to be immaterial.
Since the Stamford Lease does not provide an implicit interest rate, the Company used an annual incremental borrowing rate of
As noted above, upon adoption of ASC 842, the Company used hindsight in determining the term of the Stamford Lease. Although the Stamford Lease is renewable for
The Stamford Lease contains both a lease and non-lease component which are accounted for separately. The Company allocates the consideration to the lease and the non-lease component on a relative standalone price basis. Lease expense under ASC 842 is recognized on a straight-line basis over the lease term in the Statements of Comprehensive (Loss) Income.
There was
In June 2020, the Company entered into the Lease Amendment. The term of the Lease Amendment began when renovation of the additional space was completed and the Company took possession of the additional space in October 2020, or the Amendment Commencement Date, and ends on December 31, 2023. The Lease Amendment is also renewable for
118
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
escalations, during the lease term. The Company began paying rent for the Lease Amendment on the Amendment Commencement Date.
The Company accounted for the terms and conditions of the Lease Amendment as a lease modification, as defined in ASC 842, because it grants an additional right-of-use to an underlying asset (the new additional space). Under ASC 842, a lease modification can result in either a new lease that is accounted for separately from the original lease or as a single modified lease. The Lease Amendment is accounted for separately from the original Stamford Lease because the Lease Amendment grants the right-of-use to additional space and the price of the additional right-of-use is commensurate with its standalone price as no discounts were provided to the Company. Furthermore, there were no material changes to the original Stamford Lease.
As of the Amendment Commencement Date, the Company recorded the lease liability for the Lease Amendment as the sum of the present value of the future minimum lease payments over the term for the new lease. Since the Lease Amendment does not provide an implicit interest rate, the Company used an incremental borrowing rate of
Litigation Reserves
From time to time, the Company may become subject to arbitration, litigation or claims arising in the ordinary course of its business. Accruals are recorded when it is probable that a liability has been incurred and the amount of the liability can be reasonably estimated. The Company reviews these reserves at least quarterly and adjusts these reserves to reflect current law, progress of each case, opinions and views of legal counsel and other advisers, the Company’s experience in similar matters and intended response to the litigation. The Company expenses amounts for administering or litigating claims as incurred. Accruals for legal proceedings, if any, are included in accounts payable and accrued expenses.
Accounting Pronouncements Recently Adopted
In December 2019, the Financial Accounting Standards Board, or FASB, issued ASU No. 2019-12, Income Taxes (Topic 740), or ASU 2019-12, which removes specific exceptions to the general principles in Topic 740. ASU 2019-12 eliminates the need for an organization to analyze whether the following apply in a given period: (1) exception to the incremental approach for intra-period tax allocation; (2) exceptions to accounting for basis differences when there are ownership changes in foreign investments; and (3) exception to the general methodology for calculating income taxes in an interim period when a year-to-date loss exceeds the anticipated loss. ASU 2019-12 also simplifies the accounting for income taxes for: (i) franchise taxes that are partially based on income; (ii) transactions with a government that result in a step up in the tax basis of goodwill; (iii) separate financial statements of legal entities that are not subject to tax; and (iv) enacted changes in tax laws in interim periods. The amendments in ASU 2019-12 are effective for fiscal years, and interim periods within those fiscal years, beginning after December 15, 2020. The amendments in ASU 2019-12 related to separate financial statements of legal entities that are not subject to tax should be applied on a retrospective basis for all periods presented. The amendments related to changes in ownership of foreign equity method investments or foreign subsidiaries should be applied on a modified retrospective basis through a cumulative-effect adjustment to retained earnings as of the beginning of the fiscal year of adoption. The amendments related to franchise taxes that are partially based on income should be applied on either a retrospective basis for all periods presented or a modified retrospective basis through a cumulative-effect adjustment to retained earnings as of the beginning of the fiscal year of adoption. All other amendments should be applied on a prospective basis. The Company adopted ASU 2019-12 on January 1, 2021
119
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
and it did not have a material effect on its results of operations, financial position, and cash flows due to the full valuation allowance recorded.
Recent Accounting Pronouncements Not Yet Adopted
In October 2021, the FASB issued ASU 2021-08, Business Combinations (Topic 805), or ASU 2021-08, which requires that an entity (acquirer) recognize, and measure contract assets and contract liabilities acquired in a business combination in accordance with ASC 606. At the acquisition date, an acquirer should account for the related revenue contracts in accordance with ASC 606 as if it had originated the contracts, which should generally result in an acquirer recognizing and measuring the acquired contract assets and contract liabilities consistent with how they were recognized and measured in the acquiree’s financial statements (if the acquiree prepared financial statements in accordance with GAAP). When the acquirer is unable to assess or rely on how the acquiree applied ASC 606, the acquirer should consider the terms of the acquired contracts, such as timing of payment, identify each performance obligation in the contracts, and allocate the total transaction price to each identified performance obligation on a relative standalone selling price basis as of contract inception (i.e., the date the acquiree entered into the contracts) or contract modification to determine what should be recorded at the acquisition date. The amendments in ASU 2021-08 also provide certain practical expedients for acquirers when recognizing and measuring acquired contract assets and contract liabilities from revenue contracts in a business combination. The amendments also apply to contract assets and contract liabilities from certain other contracts to which the provisions of ASC 606 apply. The amendments in ASU 2021-08 are effective for fiscal years, and interim periods within those fiscal years, beginning after December 15, 2022. The Company will adopt ASU 2021-08 on January 1, 2023, and it does not expect it to have a material effect on its results of operations, financial position, and cash flows since the Company has no history of business acquisitions.
3. Available-for-Sale Marketable Securities
As of December 31, 2021 and 2020, the Company’s available-for-sale marketable securities consisted of debt securities issued by the U.S. Treasury, U.S. government-sponsored entities and investment grade institutions as well as municipal bonds.
The following tables summarize the Company’s available-for-sale marketable securities by major type of security as of December 31, 2021 and 2020:
As of December 31, 2021
Gross Unrealized | Estimated Fair | |||||||||||
Type of Security |
| Amortized Cost |
| Gains |
| Losses |
| Value | ||||
U.S. Treasury securities | $ | | $ | — | $ | ( | $ | | ||||
U.S. government agency obligations |
| |
| — |
| ( |
| | ||||
Corporate bonds |
| |
| — |
| ( |
| | ||||
Commercial paper | | | ( | | ||||||||
Municipal bonds |
| |
| — |
| ( |
| | ||||
Total available-for-sale marketable securities | $ | | $ | | $ | ( | $ | | ||||
120
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
As of December 31, 2020
Gross Unrealized | Estimated Fair | |||||||||||
Type of Security |
| Amortized Cost |
| Gains |
| Losses |
| Value | ||||
U.S. Treasury securities | $ | | $ | | $ | ( | $ | | ||||
U.S. government agency obligations |
| |
| |
| ( |
| | ||||
Corporate bonds |
| |
| |
| ( |
| | ||||
Commercial paper |
| |
| |
| ( |
| | ||||
Municipal bonds | | | ( | | ||||||||
Total available-for-sale marketable securities | $ | | $ | | $ | ( | $ | | ||||
The following tables summarize the fair value and gross unrealized losses of the Company’s available-for-sale marketable securities by investment category and disaggregated by the length of time that individual debt securities have been in a continuous unrealized loss position as of December 31, 2021 and 2020:
As of December 31, 2021
Less than 12 Months | 12 Months or Greater | Total | ||||||||||||||||
Gross | Gross | Gross | ||||||||||||||||
Fair | Unrealized | Fair | Unrealized | Fair | Unrealized | |||||||||||||
| Value |
| Losses |
| Value |
| Losses |
| Value |
| Losses | |||||||
U.S. Treasury securities | $ | | $ | ( | $ | — | $ | — | $ | | $ | ( | ||||||
U.S. government agency obligations |
| |
| ( |
| — |
| — |
| |
| ( | ||||||
Corporate bonds | | ( | | ( | | ( | ||||||||||||
Commercial paper | | ( | — | — | | ( | ||||||||||||
Municipal bonds |
| |
| ( |
| |
| ( |
| |
| ( | ||||||
Total | $ | | $ | ( | $ | | $ | ( | $ | | $ | ( | ||||||
As of December 31, 2020
Less than 12 Months | 12 Months or Greater | Total | ||||||||||||||||
Gross | Gross | Gross | ||||||||||||||||
Fair | Unrealized | Fair | Unrealized | Fair | Unrealized | |||||||||||||
| Value |
| Losses |
| Value |
| Losses |
| Value |
| Losses | |||||||
U.S. Treasury securities | $ | | $ | ( | $ | — | $ | — | $ | | $ | ( | ||||||
U.S. government agency obligations | | ( | — | — | | ( | ||||||||||||
Corporate bonds |
| |
| ( |
| — |
| — |
| |
| ( | ||||||
Commercial paper |
| |
| ( |
| — |
| — |
| |
| ( | ||||||
Municipal bonds |
| |
| ( |
| — |
| — |
| |
| ( | ||||||
Total | $ | | $ | ( | $ | — | $ | — | $ | | $ | ( | ||||||
As of December 31, 2021 and 2020, respectively,
As of December 31, 2021 and 2020, the Company held a total of
121
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
greater, were not considered to be material for each respective period. Based on the Company’s review of these securities, the Company believes that the cost basis of its available-for-sale marketable securities is recoverable.
U.S. Treasury and U.S. government agency obligations. The unrealized losses on the Company’s investments in direct obligations of the U.S. Treasury and government agencies were due to changes in interest rates and non-credit related factors. The contractual terms of these investments do not permit the issuer to repay principal at a price less than the amortized cost bases of the investments, which is equivalent to the par value on the maturity date. The Company expects to recover the entire amortized cost bases of these securities on the maturity date. The Company does not intend to sell these investments, and it is not more likely than not that the Company will be required to sell these investments before recovery of their amortized cost bases. The Company held
Corporate bonds, commercial paper, and municipal bonds. The unrealized losses on the Company’s investments in corporate bonds, commercial paper and municipal bonds were due to changes in interest rates and non-credit related factors. The credit ratings of these investments in the Company’s portfolio have not been downgraded below investment grade status. The contractual terms of these investments do not permit the issuer to repay principal at a price less than the amortized cost bases of the investments, which is equivalent to the par value on the maturity date. The Company expects to recover the entire amortized cost bases of these securities on the maturity date. The Company does not intend to sell these investments, and it is not more likely than not that the Company will be required to sell these investments, before recovery of their amortized cost bases. The Company held
The Company classifies its marketable debt securities based on their contractual maturity dates. As of December 31, 2021, the Company’s marketable debt securities mature at various dates through November 2024. The amortized cost and fair values of marketable debt securities by contractual maturity were as follows:
As of December 31, 2021 | As of December 31, 2020 | |||||||||||
Contractual maturity |
| Amortized Cost |
| Fair Value |
| Amortized Cost |
| Fair Value | ||||
Less than one year | $ | | $ | | $ | | $ | | ||||
One year to three years |
| |
| |
| |
| | ||||
Total | $ | | $ | | $ | | $ | | ||||
All available-for-sale marketable securities are classified as Marketable securities, current or Marketable securities, non-current depending on the contractual maturity date of the individual available-for-sale security. Other income, net includes interest and dividends, accretion/amortization of discounts/premiums, realized gains and losses on sales of securities and credit loss expense due to declines in the fair value of securities, if any. The cost of securities sold is based on the specific identification method.
During the year ended December 31, 2021, the Company sold certain shares of its available-for-sale debt securities with a total fair value of $
As of December 31, 2021 and 2020, accrued interest receivables on our available-for-sale debt securities were $
122
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
4. Accumulated Other Comprehensive (Loss) Income
The following table summarizes the changes in accumulated other comprehensive (loss) income, net of tax, from unrealized gains (losses) on available-for-sale marketable securities, the Company’s only component of accumulated other comprehensive (loss) income, for the years ended December 31, 2021, 2020 and 2019.
| Total Accumulated | ||
Other Comprehensive | |||
(Loss) Income | |||
Balance, December 31, 2018 | $ | ( | |
Other comprehensive income before reclassifications |
| | |
Amount reclassified from accumulated other comprehensive loss |
| — | |
Net current period other comprehensive income |
| | |
Balance, December 31, 2019 |
| | |
Other comprehensive income before reclassifications |
| | |
Amount reclassified from accumulated other comprehensive income |
| ( | |
Net current period other comprehensive loss |
| ( | |
Balance, December 31, 2020 | $ | | |
Other comprehensive loss before reclassifications |
| ( | |
Amount reclassified from accumulated other comprehensive income |
| ( | |
Net current period other comprehensive loss |
| ( | |
Balance, December 31, 2021 | $ | ( | |
Amounts reclassified out of accumulated other comprehensive (loss) income into net (loss) income are determined by specific identification. The reclassifications out of accumulated other comprehensive (loss) income and into net (loss) income were as follows:
Affected Line Item in the | |||||||||||
Component of Accumulated Other | Year Ended December 31, | Statements of | |||||||||
Comprehensive (Loss) Income |
| 2021 |
| 2020 |
| 2019 |
| Comprehensive (Loss) Income | |||
Unrealized gains (losses) on available-for-sale marketable securities: |
|
|
|
|
|
|
|
| |||
Realized gains on sales of securities | $ | | $ | | $ | — |
| Other income, net | |||
Income tax effect |
| |
| |
| |
| Benefit from income taxes | |||
Realized gains on sales of securities, net of tax | $ | | $ | | $ | — | |||||
5. Inventory, net
Inventories consist of the following:
| December 31, 2021 |
| December 31, 2020 | |||
Raw materials | $ | | $ | — | ||
Work-in-process |
| |
| — | ||
Total | $ | | $ | — | ||
As of December 31, 2021, inventory balances include inventory costs subsequent to regulatory approval of KORSUVA injection on August 23, 2021. For the year ended December 31, 2021,
123
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
were expensed as incurred. There were
6. Prepaid Expenses
As of December 31, 2021, the amount of prepaid expenses was $
7. Property and Equipment, net
Property and equipment, net consists of the following:
December 31, | ||||||
| 2021 |
| 2020 | |||
Computer and office equipment | $ | | $ | | ||
Laboratory equipment |
| — |
| | ||
Furniture and fixtures |
| |
| | ||
Leasehold improvements |
| |
| | ||
$ | | $ | | |||
Less accumulated depreciation and amortization |
| |
| | ||
Property and equipment, net | $ | | $ | | ||
Depreciation and amortization expense included in R&D expense and G&A expense was $
During the year ended December 31, 2021, the Company sold laboratory equipment that was fully depreciated, which resulted in gains on sales of property and equipment of $
8. Restricted Cash
The Company is required to maintain a stand-by letter of credit as a security deposit under its leases for its office space in Stamford, Connecticut (refer to Note 18, Commitments and Contingencies: Leases). The fair value of the letter of credit approximates its contract value. The Company’s bank requires the Company to maintain a restricted cash balance to serve as collateral for the letter of credit issued to the landlord by the bank. As of December 31, 2021, the restricted cash balance for the Stamford Lease was invested in a commercial money market account.
As of December 31, 2021 and 2020, the Company had $
124
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
The following table provides a reconciliation of cash, cash equivalents and restricted cash reported within the Balance Sheets that sum to the total of the same such amounts shown in the Statements of Cash Flows.
| December 31, 2021 |
| December 31, 2020 | |||
Cash and cash equivalents | $ | | $ | | ||
Restricted cash, long-term assets |
| |
| | ||
Total cash, cash equivalents, and restricted cash shown in the Statements of Cash Flows | $ | | $ | | ||
9. Accounts Payable and Accrued Expenses
Accounts payable and accrued expenses consist of the following:
| December 31, 2021 |
| December 31, 2020 | |||
Accounts payable | $ | | $ | | ||
Accrued research projects |
| |
| | ||
Accrued compensation and benefits |
| |
| | ||
Accrued professional fees and other |
| |
| | ||
Total | $ | | $ | | ||
10. Stockholders’ Equity
The Company’s Board of Directors has authorized
Each share of common stock entitles the holder to
In October 2021, the Company issued
In August 2021, as a result of the achievement of certain performance targets, an aggregate of
In June 2021, as a result of the completion of the
In February and March 2021, as a result of the achievement of certain performance targets, an aggregate of
125
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
In February 2021, as a result of the completion of the first year of the
In December 2020, as a result of the achievement of a performance target, an aggregate of
In October 2020, the Company issued
Pursuant to the stock purchase agreement with Vifor, or the Vifor Purchase Agreement, Vifor will not, and will not cause any direct or indirect affiliate to, during the period beginning on October 15, 2020 and ending at the close of business on October 15, 2022, or the Restricted Period, (i) offer, pledge, sell, contract to sell, sell any option or contract to purchase, purchase any option or contract to sell, grant any option, right or warrant to purchase, lend, or otherwise transfer or dispose of, directly or indirectly, any shares of common stock of the Company or any securities convertible into or exercisable or exchangeable for common stock of the Company (including without limitation, common stock or such other securities which may be deemed to be beneficially owned by Vifor in accordance with the rules and regulations of the SEC and securities which may be issued upon exercise of a stock option or warrant) owned by Vifor as of the date hereof or acquired prior to the end of the Restricted Period (collectively with the common stock, referred to as the Lock-Up Securities), except any such sale, option or contract by and between Vifor and one of its affiliates (including Vifor Pharma Group Ltd. or VFMCRP), (ii) enter into any hedging, swap or other agreement or transaction that transfers, in whole or in part, any of the economic consequences of ownership of the Lock-Up Securities, whether any such transaction described in clause (i) or (ii) above is to be settled by delivery of Lock-Up Securities, in cash or otherwise, (iii) make any demand for or exercise any right with respect to the registration of any Lock-Up Securities, or (iv) publicly disclose the intention to do any of the foregoing.
Under the Vifor Purchase Agreement, the parties also agreed that, in certain circumstances, upon the request of Vifor, the parties will enter into a registration rights agreement prior to the end of the Restricted Period that would provide Vifor (or its affiliate transferee) customary registration rights with respect to the shares of common stock issued pursuant to the Vifor Purchase Agreement following the expiration of the Restricted Period.
In June 2020, as a result of the completion of the
In April and June 2020, as a result of the achievement of certain performance targets, an aggregate of
In December 2019, as a result of the achievement of a clinical performance target, restricted stock units of various executive officers vested and were converted into
In August 2019, the Company entered into a Non-Exclusive License Agreement, or the Enteris License Agreement, with Enteris Biopharma, Inc., or Enteris (see Note 18, Commitments and Contingencies for additional information regarding the Enteris License Agreement). As consideration for the licensed rights under the Enteris License Agreement, the Company paid an upfront fee equal to $
126
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
into a Common Stock Purchase Agreement, or the Enteris Purchase Agreement, with Enteris and its affiliate, EBP Holdco LLC, collectively referred to as Purchaser, pursuant to which the Company issued and sold to Purchaser
In July 2019, the Company entered into an underwriting agreement with J.P. Morgan Securities LLC and Jefferies LLC, as representatives of the several underwriters named therein, relating to the issuance and sale by the Company of
This offering was made pursuant to the Company’s Shelf Registration Statement on Form S-3 (File No. 333-230333), or the Shelf Registration Statement, filed with the SEC on March 15, 2019 and declared effective on April 4, 2019, and a related prospectus supplement dated July 24, 2019, which was filed with the SEC on July 25, 2019. The Shelf Registration Statement provides for aggregate offerings of up to $
In May 2019, as a result of the achievement of a clinical performance target, an aggregate of
In March 2019, the Company entered into a consulting agreement with an existing stockholder. In accordance with the agreement, the stockholder provided various consulting services to the Company in exchange for
127
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
11. Fair Value Measurements
The following tables summarize the Company’s financial assets measured at fair value on a recurring basis as of December 31, 2021 and 2020 and by level within the fair value hierarchy:
Fair value measurement as of December 31, 2021:
Quoted prices in | Significant other | Significant | ||||||||||
Financial assets | active markets for | observable | unobservable | |||||||||
identical assets | inputs | inputs | ||||||||||
Type of Instrument |
| Total |
| (Level 1) |
| (Level 2) |
| (Level 3) | ||||
Cash and cash equivalents: |
|
|
|
|
|
|
|
| ||||
Money market funds and checking accounts | $ | | $ | | $ | — | $ | — | ||||
Available-for-sale marketable securities: |
|
|
|
|
| |||||||
U.S. Treasury securities |
| |
| — |
| |
| — | ||||
U.S. government agency obligations |
| |
| — |
| |
| — | ||||
Corporate bonds |
| |
| — |
| |
| — | ||||
Commercial paper |
| |
| — |
| |
| — | ||||
Municipal bonds |
| |
| — |
| |
| — | ||||
Restricted cash: |
|
|
|
|
| |||||||
Commercial money market account |
| |
| |
| — |
| — | ||||
Total financial assets | $ | | $ | | $ | | $ | — | ||||
Fair value measurement as of December 31, 2020:
Quoted prices in | Significant other | Significant | ||||||||||
Financial assets | active markets for | observable | unobservable | |||||||||
identical assets | inputs | inputs | ||||||||||
Type of Instrument |
| Total |
| (Level 1) |
| (Level 2) |
| (Level 3) | ||||
Cash and cash equivalents: |
|
|
|
|
|
|
|
| ||||
Money market funds and checking accounts | $ | | $ | | $ | — | $ | — | ||||
Available-for-sale marketable securities: |
|
|
|
|
|
|
|
| ||||
U.S. Treasury securities | | — | | — | ||||||||
U.S. government agency obligations |
| |
| — |
| |
| — | ||||
Corporate bonds |
| |
| — |
| |
| — | ||||
Commercial paper |
| |
| — |
| |
| — | ||||
Municipal bonds | | — | | — | ||||||||
Restricted cash: |
|
|
|
|
|
|
|
| ||||
Commercial money market account |
| |
| |
| — |
| — | ||||
Total financial assets | $ | | $ | | $ | | $ | — | ||||
There were
128
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
12. Collaboration and Licensing Agreements
Vifor (International) Ltd. (Vifor)
In October 2020, the Company entered into a license agreement with Vifor, or the Vifor Agreement, under which the Company granted Vifor an exclusive license solely in the United States to use, distribute, offer for sale, promote, sell and otherwise commercialize difelikefalin injection for all therapeutic uses relating to the inhibition, prevention or treatment of itch associated with pruritus in hemodialysis and peritoneal dialysis patients in the United States. Under the Vifor Agreement, the Company retains all rights with respect to the clinical development of, and activities to gain regulatory approvals of, difelikefalin injection in the United States. The Joint Commercialization Committee, or JCC, have the responsibility for overall coordination and oversight of Vifor (and any affiliates or sublicensees). The Company’s membership on the JCC is at its sole discretion and is not its obligation.
The Vifor Agreement provides full commercialization rights in dialysis clinics to Vifor in the United States under a profit-sharing arrangement. Pursuant to the profit-sharing arrangement, the Company will generally be entitled to
The Company has identified
Under the terms of the Vifor Agreement, the Company received from Vifor an upfront payment of $
In addition, pursuant to the Vifor Agreement, the Company is eligible to receive payments of up to $
At inception of the Vifor Agreement, the transaction price of $
After U.S. regulatory approval of KORSUVA injection in August 2021, the Company received an additional $
129
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
shares at the closing price of the Company’s common stock on the date of the achievement of the milestone of $
The license also requires Vifor to promote and take orders for difelikefalin injection, or Licensed Product, throughout the United States, including coordinating with VFMCRP promotional activities to FMC U.S. Dialysis Clinics which are subject to the Company’s rights under the VFMCRP Agreement. The license also allows Vifor to grant sub-licenses, which, in certain cases, requires the Company’s prior written consent. The Company retains the rights to import, distribute, promote, sell and otherwise commercialize the Licensed Product on an exclusive basis outside of the Field either in or outside of the United States.
The Company retains the rights to make and have made the Licensed Product, on a non-exclusive basis, in the United States for commercial sale of the Licensed Product for use for all therapeutic uses to prevent, inhibit or treat itch associated with pruritus in hemodialysis and peritoneal-dialysis patients, or the Field, anywhere in the world and for supply of Licensed Product to Vifor under the terms of a supply agreement, or the Vifor Supply Agreement, which was executed in September 2021. The supply price is the Company’s COGS, as calculated under GAAP, plus an agreed upon margin. The Vifor Supply Agreement will co-terminate with the Vifor Agreement.
The Vifor Supply Agreement is accounted for as a customer option that is not a material right because the selling price of the Licensed Product under the Vifor Supply Agreement is the Company’s COGS plus an agreed upon margin, which is commensurate with the “COGS plus” model that the Company would charge other parties under similar agreements (the standalone selling price) and not at a discount. Therefore, the sale of commercial supply to Vifor is not a performance obligation under the Vifor Agreement but rather the Vifor Supply Agreement is a separate agreement from the Vifor Agreement. The only performance obligation under the Vifor Supply Agreement is the delivery of the Licensed Product to Vifor for commercialization. Revenue from the sale of the Licensed Product to Vifor will be recognized in the Company’s Statements of Comprehensive (Loss) Income as sales of the Licensed Product occur. The Company had commercial supply revenue of $
The Vifor Agreement will continue in effect until its expiration upon the cessation of commercial sale of difelikefalin injection in the United States by Vifor and its affiliates and sublicensees, or until the earlier termination of the Vifor Agreement.
The Vifor Agreement may be terminated earlier by either party for material breach that is not cured within
Vifor Fresenius Medical Care Renal Pharma Ltd. (VFMCRP)
In May 2018, the Company entered into a license agreement, or the VFMCRP Agreement, with VFMCRP under which the Company granted VFMCRP an exclusive, royalty-bearing license, or the VFMCRP License, to seek regulatory approval to commercialize, import, export, use, distribute, offer for sale, promote, sell and otherwise commercialize the Licensed Product in the Field worldwide (excluding the United States, Japan and South Korea), or the Territory. VFMCRP cannot perform development activities on their own unless specifically allocated to VFMCRP by
130
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
the Joint Development Committee, or JDC, and Joint Steering Committee, or JSC. The Company’s membership on the JSC or JDC is at its sole discretion and is not its obligation.
The Company is responsible, at its own cost, to undertake clinical and non-clinical development, or the R&D services. The Company is also responsible to provide all content and subject matter expertise required for registration with the European Medicines Agency, or EMA, in the European Union, or the EU, that will be needed by VFMCRP for such registration, including participation in regulatory meetings, as needed. VFMCRP will contribute, at its own cost, its clinical development expertise as reasonably useful for such development activities, such as preparing the clinical results that the Company presents to it in a format acceptable to the EMA to obtain marketing approval in the EU.
The Company has identified
The
Upon entry into the VFMCRP Agreement, VFMCRP made a non-refundable, non-creditable $
At inception of the VFMCRP Agreement, the transaction price of $
After U.S. regulatory approval of KORSUVA injection in August 2021, the Company was entitled to receive a $
131
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
The Company is eligible to receive from VFMCRP additional regulatory and commercial milestone payments in the aggregate of up to $
At inception of the VFMCRP Agreement, there was significant uncertainty as to whether marketing approval would be obtained in the Territory for the Licensed Product. Therefore, at that time, there was a significant probability that any potential revenue from sales of the Licensed Product that would be included in the transaction price would be reversed when the uncertainty is resolved. Consequently, any sales royalties and sales milestones are constrained from the transaction price at inception of the VFMCRP Agreement and will be recognized as revenue if, and when, such sales transactions occur in the future.
The license also requires VFMCRP to promote and take orders in the U.S. for sale by the Company to FMC U.S. Dialysis Clinics and allows VFMCRP to grant sub-licenses, which, in certain cases, requires the Company’s prior written consent. The Company retains the rights to import, distribute, promote, sell and otherwise commercialize the Licensed Product outside of the Field and outside of the Territory.
The Company retains the rights to make and have made the Licensed Product in the Territory for commercial sale by VFMCRP in the Field in or outside the Territory and for supply of Licensed Product to VFMCRP under the terms of a supply agreement, or the VFMCRP Supply Agreement, which was executed in May 2020. The supply price is the Company’s COGS, as calculated under U.S. GAAP, plus an agreed upon margin. The VFMCRP Supply Agreement will co-terminate with the VFMCRP Agreement.
The VFMCRP Supply Agreement is accounted for as a customer option that is not a material right because the selling price of the Licensed Product under the VFMCRP Supply Agreement is the Company’s COGS plus an agreed upon margin, which is commensurate with the “COGS plus” model that the Company would charge other parties under similar agreements (the standalone selling price) and not at a discount. Therefore, the sale of clinical compound to VFMCRP is not a performance obligation under the VFMCRP Agreement but rather the VFMCRP Supply Agreement is a separate agreement from the VFMCRP Agreement. The only performance obligation under the VFMCRP Supply Agreement is the delivery of the Licensed Product to VFMCRP for commercialization. Revenue from the sale of the Licensed Product to VFMCRP will be recognized in the Company’s Statements of Comprehensive (Loss) Income as sales of the Licensed Product occur. During the years ended 2021 and 2020, the Company recognized clinical compound revenue of $
The VFMCRP Agreement terminates upon the expiration of all royalty terms with respect to the Licensed Products, which expire on a Product-by-Product and country-by-country basis, at the latest of (a) the expiration of all patent rights licensed to VFMCRP covering such Licensed Product; (b) the expiration of all regulatory and data exclusivity applicable to such Licensed Product in such country and (c) the tenth anniversary of the first commercial sale of such Product in such country.
The VFMCRP Agreement may be terminated earlier by either party for material breach that is not cured within
132
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
upon the earlier of (1) the acceptance for filing of an NDA covering Licensed Product filed with the FDA (after completion of the Phase 3 program) or (2) the third anniversary of the Effective Date, the VFMCRP Agreement may be terminated by VFMCRP in its entirety or with respect to any countries within the Territory upon written notice to the Company. Such termination will be effective
If the VFMCRP Agreement terminates early for any reason stated above, VFMCRP’s licenses will terminate, VFMCRP’s rights to use the Company’s confidential information and the Company’s know-how will revert to the Company and VFMCRP will assign and transfer to the Company all right, title and interest in all regulatory applications (IND’s and NDA’s), regulatory approval applications and regulatory approvals in the Territory covering Licensed Product.
Maruishi Pharmaceutical Co., Ltd. (Maruishi)
In April 2013, the Company entered into a license agreement with Maruishi, or the Maruishi Agreement, under which the Company granted Maruishi an exclusive license to develop, manufacture, and commercialize drug products containing difelikefalin for acute pain and/or uremic pruritus in Japan. Maruishi has the right to grant sub-licenses in Japan, which entitles the Company to receive sub-license fees, net of prior payments made by Maruishi to the Company. Under the Maruishi Agreement, the Company and Maruishi are required to use commercially reasonable efforts, at their own expense, to develop, obtain regulatory approval for and commercialize difelikefalin in the United States and Japan, respectively. In addition, the Company provided Maruishi specific clinical development services for difelikefalin used in Maruishi’s field of use.
Under the Maruishi Agreement, the Company identified
Under the terms of the Maruishi Agreement, the Company is eligible to receive milestone payments upon the achievement of defined clinical and regulatory events as well as tiered, low double-digit royalties with respect to any sales of the licensed product sold in Japan by Maruishi, if any, and share in any sub-license fees.
During the years ended December 31, 2021, 2020 and 2019, the Company recognized clinical compound revenue of $
The Company incurred R&D expense related to the Maruishi Agreement of $
Chong Kun Dang Pharmaceutical Corporation (CKDP)
In April 2012, the Company entered into a license agreement, or the CKDP Agreement with CKDP in South Korea, under which the Company granted CKDP an exclusive license to develop, manufacture and commercialize drug products containing difelikefalin in South Korea. The Company and CKDP are each required to use commercially reasonable efforts, at their respective expense, to develop, obtain regulatory approval for and commercialize difelikefalin in the United States and South Korea, respectively. The Company identified the granting of the license as its only performance obligation under the CKDP Agreement.
133
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Under the terms of the CKDP Agreement, the Company is eligible to receive milestone payments upon the achievement of defined clinical and regulatory events as well as tiered royalties, with percentages ranging from the high single digits to the high teens, based on net sales of products containing difelikefalin in South Korea, if any, and share in any sub-license fees.
13. Revenue Recognition
The Company currently recognizes revenue in accordance with ASC 606, as amended, for the Vifor, VFMCRP, Maruishi and CKDP agreements (see Note 12, Collaboration and Licensing Agreements). Under each of these agreements, the Company has recognized revenue from (1) commercial supply sales to Vifor under the Vifor Supply Agreement; (2) upfront payments; (3) regulatory milestone payments under the Vifor and VFMCRP agreements; and (4) clinical development milestone payments under the Maruishi and CKDP agreements. The Company has also recognized revenue from a sub-license payment earned under the Maruishi Agreement. Under the Maruishi and CKDP agreements, the Company may earn additional future milestone payments upon the achievement of defined clinical events, and under the VFMCRP, Maruishi and CKDP agreements, upon the achievement of defined regulatory events, and under the Vifor, VFMCRP and Maruishi agreements, from sales milestones. The Company may also recognize revenue in the future from royalties on net sales under the VFMCRP, Maruishi and CKDP agreements. In addition, the Company has recognized revenue upon the delivery of clinical compound to VFMCRP and Maruishi in accordance with separate supply agreements.
For the year ended December 31, 2021, the Company had license and collaboration agreements with Vifor, VFMCRP, Maruishi and CKDP. The following table provides amounts included in the Company’s Statements of Comprehensive (Loss) Income as revenue for the years ended December 31, 2021, 2020 and 2019:
Year Ended December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
License and milestone fees | |||||||||
VFMCRP | $ | | $ | | $ | | |||
Vifor | | | — | ||||||
Maruishi | | — | — | ||||||
CKDP | — | | — | ||||||
Total license and milestone fees | $ | | $ | | $ | | |||
Collaborative revenue | |||||||||
Maruishi | $ | | $ | — | $ | — | |||
Total Collaborative revenue | $ | | $ | — | $ | — | |||
Commercial supply revenue | |||||||||
Vifor (KORSUVA injection) | $ | | $ | — | $ | — | |||
Total commercial supply revenue | $ | | $ | — | $ | — | |||
Clinical compound revenue | |||||||||
VFMCRP (difelikefalin injection) | $ | | $ | | $ | — | |||
Maruishi | | | | ||||||
Total clinical compound revenue | $ | | $ | | $ | | |||
Contract balances
As of December 31, 2021 and 2020, there were
134
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
The Company routinely assesses the creditworthiness of its license and collaboration partners. The Company has not experienced any losses related to receivables from its license or collaboration partners during the years ended December 31, 2021, 2020, or 2019.
Performance obligations
Under the Vifor Agreement, the Company’s only performance obligation is granting a license to allow Vifor to commercialize difelikefalin in the United States, which occurred at inception of the contract in October 2020 (see Note 12, Collaboration and Licensing Agreements).
Under the Vifor Supply Agreement, the Company’s only performance obligation is the delivery of KORSUVA injection to Vifor in accordance with the receipt of purchase orders.
Under the VFMCRP Agreement, the Company’s performance obligations of granting a license to allow VFMCRP to commercialize difelikefalin injection worldwide, except in the United States, Japan and South Korea, which occurred at inception of the contract in May 2018, and performing R&D services by the Company to obtain sufficient clinical data which will be shared with VFMCRP to allow them to receive regulatory approval to sell difelikefalin in the licensed territory, are not distinct, and are accounted for as a single performance obligation during the period that the R&D services are rendered (see Note 12, Collaboration and Licensing Agreements).
The Company’s distinct performance obligations under the Maruishi Agreement include transfer of the license to the Company’s IP, which allowed Maruishi to develop and commercialize difelikefalin, for acute pain and uremic pruritus indications in Japan, which occurred at inception of the contract in 2013, and performance of R&D services, which occurred from 2013 to 2015, as those services were rendered. The Company agreed to conduct limited work on an oral tablet formulation of difelikefalin and to conduct Phase 1 and proof-of-concept Phase 2 clinical trials of an intravenous formulation of difelikefalin to be used to treat patients with uremic pruritus. The Company agreed to transfer the data and information from such development to Maruishi for its efforts to obtain regulatory approval in Japan. These activities are referred to as R&D services (see Note 12, Collaboration and Licensing Agreements).
The Company’s only performance obligation under the supply agreement with Maruishi is to deliver clinical compound to Maruishi in accordance with the receipt of purchase orders. The Company’s only performance obligation under the VFMCRP Supply Agreement is to deliver difelikefalin injection to VFMCRP in accordance with the receipt of purchase orders.
Under the CKDP Agreement, the Company’s only performance obligation is to transfer the license to the Company’s IP related to difelikefalin.
Upon execution of the Vifor, VFMCRP, Maruishi and CKDP agreements, the Company received a single fixed payment from each counterparty in exchange for granting the respective licenses and performing its other obligations (if applicable). In addition, each of the counterparties made an equity investment in the Company’s common stock.
Transaction price allocated to the remaining performance obligations
At inception of the Vifor Agreement, the entire transaction price of $
135
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
At inception of the VFMCRP Agreement, the entire transaction price of $
As of December 31, 2021, there were
Significant judgments
In applying ASC 606, as amended, to its
1. | Determination of the number of distinct performance obligations in a contract |
The VFMCRP Agreement contains
The Maruishi Agreement contains
In addition, the Company’s promise in the Maruishi contract to transfer the license is separately identifiable from the promise to provide defined R&D services (i.e., distinct within the context of the contract) because the Company is not using the goods or services as inputs to produce or deliver the combined output or outputs specified by the customer. The combined output specified by Maruishi is its right to conduct development activities related to difelikefalin in Japan, which could result in regulatory approval in Japan. That right is derived from the Company’s grant of the license. Maruishi is conducting clinical trials on its own and does not require the R&D services provided by the Company. Furthermore, the R&D services do not significantly modify or customize the license and vice versa. Finally, the license and R&D services are not highly interdependent or highly interrelated because the Company is able to fulfill its promise to transfer the initial license independently from its promise to subsequently provide the R&D services, which Maruishi can obtain on its own.
The only performance obligation in the Vifor and CKDP agreements is the granting of the license. The only performance obligation in the Vifor Supply Agreement is the delivery of KORSUVA injection to Vifor.
136
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
2. | Determination of the transaction price, including whether any variable consideration is included at inception of the contract |
The transaction price is the amount of consideration that the Company expects to be entitled to in exchange for transferring promised goods or services to the customer. The transaction price must be determined at inception of a contract and may include amounts of variable consideration. However, there is a constraint on inclusion of variable consideration, such as milestone payments or sales-based royalty payments, in the transaction price related to licenses of IP, if there is uncertainty at inception of the contract as to whether such consideration will be recognized in the future (see Note 2, Summary of Significant Accounting Policies: Revenue Recognition).
The decision as to whether or not it is probable that a significant reversal of revenue will occur in the future, depends on the likelihood and magnitude of the reversal and is highly susceptible to factors outside the entity’s influence (for example, the Company cannot determine the outcome of clinical trials; the Company cannot determine if or when they or the counterparty will initiate or complete clinical trials; and the Company’s ability to obtain regulatory approval is difficult). In addition, the uncertainty is not expected to be resolved for a long period of time (in the order of years) and finally, the Company has limited experience in the field.
Therefore, at inception of the Vifor, VFMCRP, Maruishi and CKDP agreements, milestones and sales-based royalty payments were not included in the transaction price based on the factors noted above.
Under the Vifor Agreement, the
Under the VFMCRP Agreement, the single combined performance obligation was satisfied as the R&D services were rendered and the transaction price (including the upfront payment of $
All performance obligations under the Maruishi Agreement and the CKDP Agreement were satisfied by the end of 2015. In the future, any milestone event will be recognized in accordance with Note 2, Significant Accounting Polices: Revenue Recognition, as milestone and license fee revenue and collaboration revenue based upon the relative standalone selling prices of the
Under the Maruishi Agreement, the transaction price includes only the non-refundable and non-creditable upfront license fee of $
137
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Under the CKDP Agreement, the transaction price includes only the non-refundable and non-creditable upfront license fee of $
3. | Determination of the estimate of the standalone selling price of performance obligations |
In order to recognize revenue under ASC 606, as amended, for contracts for which more than one distinct performance obligation has been identified, the Company must allocate the transaction price to the performance obligations based upon their standalone selling prices. The best evidence of standalone selling price is an observable price of a good or service when sold separately by an entity in similar circumstances to similar customers. If such evidence is not available, standalone selling price should be estimated so that the amount that is allocated to each performance obligation equals the amount that the entity expects to receive for transferring goods or services. The Company has identified more than one performance obligation only in the Maruishi Agreement. Since evidence based on observable prices is not available for the performance obligations under the Maruishi Agreement, the Company considered market conditions and entity-specific factors, including those contemplated in negotiating the agreements, as well as certain internally developed estimates.
At inception of the Maruishi Agreement, the Company determined the estimate of standalone selling price for the license performance obligation by using the adjusted market assessment approach. Under this method, the Company forecasted and analyzed difelikefalin in the Japanese market, the phase of clinical development as well as considered recent similar license arrangements within the same phase of clinical development, therapeutic area, type of agreement, etc. To estimate the standalone selling price of the R&D services, the Company forecasted its expected costs of satisfying that performance obligation and added a margin for that service.
4. | Determination of the method of allocation of the transaction price to the distinct performance obligations |
At inception of the Maruishi Agreement, the Company allocated the transaction price of $
Since the Vifor, VFMCRP and agreements each contain only
5. | Determination of the timing of revenue recognition for contracts |
Revenue should be recognized when, or as, an entity satisfies a performance obligation by transferring a promised good or service to a customer; i.e., when the customer obtains control of the good or service. The licenses granted to Vifor, Maruishi and CKDP are being accounted for as distinct performance obligations. As discussed below, the licenses
138
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
relate to functional IP for which revenue is recognized at a point in time – in the case of these
The licenses grant Vifor, Maruishi and CKDP the right to use the Company’s IP relating to difelikefalin as it existed at the point in time that the licenses were granted. That IP has significant standalone functionality as it provides the customer with the ability to perform a function or task, such as to manufacture difelikefalin, conduct clinical trials, or commercialize difelikefalin, and is considered to be functional IP.
During the license periods, the Company is continuing to develop and advance difelikefalin by conducting clinical trials. Those development efforts are for its own benefit and do not substantively change the significant standalone functionality of the licensed IP granted to Vifor, Maruishi or CKDP. Therefore, the Company’s ongoing development efforts do not significantly affect the IP’s utility to which Vifor, Maruishi or CKDP have rights. Furthermore, if the Company abandons its development efforts, Vifor, Maruishi or CKDP may still continue to develop difelikefalin in their respective countries.
The R&D services performance obligation under the Maruishi Agreement represents a separate performance obligation. The R&D services were provided to Maruishi by the Company from inception of the agreement in 2013 through the third quarter of 2015, at which time the Company had fulfilled its promise related to the R&D services. Revenue related to the R&D services performance obligation was recognized as services were performed based on the costs incurred as a percentage of the estimated total costs to be incurred to complete the performance obligation.
Similarly, under the VFMCRP Agreement, revenue related to the single distinct performance obligation, which includes both granting of the license and performance of the R&D services, was recognized as the R&D services were performed, based on the costs incurred as a percentage of the estimated total costs to be incurred to complete the performance obligation. As of December 31, 2021, there is
Under the Vifor Supply Agreement, revenue from the sales of KORSUVA injection are recognized in the Company’s Statements of Comprehensive (Loss) Income as sales of KORSUVA injection occurs and control is transferred to Vifor.
6. | Determination of consideration as variable consideration, including factors related to inclusion in the transaction price at inception of the contract and timing of recognition as revenue. |
The Vifor, VFMCRP, Maruishi and CKDP agreements contain potential payments related to achievement of defined milestone events and royalties (excluding Vifor) upon net sales of future products, which are considered to be variable consideration because of the uncertainty of occurrence of any of those events specified in those agreements at inception of the agreements. Therefore, those potential payments were not included in the transaction price at the inception of the agreements.
Revenue related to achievement of milestone events is recognized when the Company has determined that it is probable that a milestone event will be achieved and there will not be a significant reversal of revenue in future periods. Upon probability of achievement of a milestone event, the most likely amount of variable consideration is included in the transaction price. Subsequent changes to the transaction price, after contract initiation, are allocated to the performance obligations in the contract on the same basis as at contract inception. Revenue for variable consideration is recognized in the same manner (point in time or over time) as for the performance obligations to which the payment amounts were allocated.
139
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
The Maruishi Agreement and the CKDP Agreement specify that certain development milestones will be achieved at pre-specified defined phases of a clinical trial (such as initiation or completion or other pre-specified time during a clinical trial as specified in the agreements).
After U.S. regulatory approval of KORSUVA injection in August 2021, the Company received an additional $
After U.S. regulatory approval of KORSUVA injection in August 2021, the Company received a $
In January 2021, the criteria for revenue recognition for a milestone event set forth in the Maruishi Agreement was achieved, and the Company recorded $
During the year ended December 31, 2020, the criteria for revenue recognition for a milestone event set forth in the CKDP Agreement was achieved, and the Company recorded $
Sublicense payments
Vifor’s, VFMCRP’s, Maruishi’s and CKDP’s right to grant sub-licenses is explicitly stated in their respective license agreements. The amount of any potential sub-license fees to be received by the Company, which is based on a formula if applicable to that respective agreement, is considered to be variable consideration and is constrained from inclusion in the transaction price at inception of the contract since at that time it was probable that there would be a reversal of such revenue in the future because the Company did not know if a sublicense would be granted in the future.
Sales-based Royalty Payments
The VFMCRP Agreement, CKDP Agreement and Maruishi Agreement each allow the Company to earn sales-based royalty payments in exchange for a license of intellectual property. In that case, the Company will recognize revenue for a sales-based royalty only when (or as) the later of the following events occurs:
| a. | The subsequent sale or usage occurs. |
| b. | The performance obligation to which some or all of the sales-based royalty has been allocated has been satisfied (or partially satisfied). |
Since the sale (item a, above) occurs after the license was delivered (item b, above), the sales-based royalty exception, to exclude such royalty payments from the transaction price, applies to the overall revenue stream. Therefore,
140
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
sales-based royalty payments are recognized as revenue when the customer’s sales occur. To date,
14. Stock-Based Compensation
2019 Inducement Plan
In October 2019, the Company’s Board of Directors adopted the 2019 Inducement Plan, or the 2019 Plan, which is a non-stockholder approved stock plan adopted pursuant to the “inducement exception” provided under Nasdaq Listing Rule 5635(c)(4), or Rule 5635, for the purpose of awarding (i) non-statutory stock options, (ii) restricted stock awards, (iii) restricted stock unit awards, (iv) other stock awards (collectively, the Inducement Awards) to new employees of the Company, as inducement material to such new employees entering into employment with the Company. On November 20, 2019, the Company filed a Registration Statement on Form S-8 with the SEC covering the offering of up to
2014 Equity Incentive Plan
The Company’s 2014 Equity Incentive Plan, or the 2014 Plan, is administered by the Company’s Board of Directors or a duly authorized committee thereof, referred to as the Plan administrator. The 2014 Plan provides for the grant of incentive stock options, non-statutory stock options, restricted stock awards, restricted stock unit awards, stock appreciation rights, performance stock awards and other forms of equity compensation, collectively referred to as Stock Awards. Additionally, the 2014 Plan provides for the grant of performance cash awards. Incentive stock options may be granted only to employees. All other awards may be granted to employees, including officers, non-employee directors, and consultants.
The aggregate number of shares of the Company’s common stock reserved for issuance under the 2014 Plan has automatically increased on January 1 of each year, beginning on January 1, 2015 and will continue to increase on January 1 of each year through and including January 1, 2024, by
141
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Restricted Stock Units
On December 17, 2021, the Compensation Committee of the Company’s Board of Directors approved and granted a total of
On October 29, 2021, the Compensation Committee of the Company’s Board of Directors also approved and granted
Pursuant to the Company’s non-employee director compensation policy, an aggregate of
On March 30, 2021, the Compensation Committee of the Company’s Board of Directors approved and granted a total of
Additionally on March 30, 2021, the Compensation Committee of the Company’s Board of Directors also approved and granted a total of
142
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
of restricted stock units on November 1, 2021 (see Stock Award Modifications below). As of December 31, 2021,
Pursuant to the Company’s non-employee director compensation policy, an aggregate of
In February 2020, the Compensation Committee of the Company’s Board of Directors approved and granted a total of
Additionally in February 2020, the Compensation Committee of the Company’s Board of Directors also approved and granted a total of
Pursuant to the terms of the Company’s non-employee director compensation policy, an aggregate of
143
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
In March 2019, the Compensation Committee of the Company’s Board of Directors approved and granted a total of
A summary of restricted stock unit activity related to employees and non-employee members of the Company’s Board of Directors as of and for the year ended December 31, 2021 is as follows:
Weighted | |||||
Number of | Average Grant | ||||
| Units |
| Date Fair Value | ||
Outstanding, December 31, 2020 |
| | $ | | |
Awarded |
| |
| | |
Vested and released |
| ( |
| | |
Outstanding, December 31, 2021 |
| | $ | | |
Restricted stock units exercisable (vested and deferred), December 31, 2021 |
| — | |||
144
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Stock Options
A summary of the Company’s stock option activity related to employees, non-employee members of the Board of Directors and non-employee consultants for the 2019 Plan and the 2014 Plan as of and for the year ended December 31, 2021 is as follows:
Weighted | Aggregate | |||||||
Number of | Average Exercise | Intrinsic | ||||||
| Shares |
| Price |
| Value | |||
Outstanding, December 31, 2020 |
| | $ | |
|
| ||
Granted |
| |
| |
|
| ||
Exercised |
| ( |
| |
|
| ||
Forfeited |
| ( |
| |
|
| ||
Expired |
| ( |
| |
|
| ||
Outstanding, December 31, 2021 |
| | $ | | $ | | ||
Weighted average remaining contractual life as of December 31, 2021 (in years) |
|
|
|
|
| |||
Options exercisable, December 31, 2021 |
| | $ | | $ | | ||
Weighted average remaining contractual life as of December 31, 2021 (in years) |
|
|
|
|
| |||
Options vested and expected to vest as of December 31, 2021 |
| | $ | | $ | | ||
Weighted average remaining contractual life as of December 31, 2021 (in years) |
|
|
|
|
| |||
The total fair value of options vested during the years ended December 31, 2021, 2020 and 2019 was $
During the years ended December 31, 2021, 2020 and 2019, the Company granted
| |||||||
Year Ended December 31, | |||||||
| 2021 |
| 2020 |
| 2019 |
| |
Risk-free interest rate |
| % | % | % | |||
Expected volatility |
| % | % | % | |||
Expected dividend yield |
| % | % | % | |||
Expected life of employee and Board options (in years) |
|
|
| ||||
The weighted average grant date fair value of options granted to employees and non-employee members of the Board of Directors for their Board service during the years ended December 31, 2021, 2020 and 2019 was $
145
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
During the years ended December 31, 2021, 2020 and 2019, the Company recognized compensation expense relating to stock options as follows:
Year Ended December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
Research and development | $ | | $ | | $ | | |||
General and administrative |
| |
| |
| | |||
Total stock option expense | $ | | $ | | $ | | |||
The following were excluded from the table above as they are not related to stock options: compensation expense for i) the vesting of executives’ restricted stock units for $
As of December 31, 2021, the total compensation expense relating to unvested options granted to employees and non-employee members of the Board of Directors that had not yet been recognized was $
The Company does not expect to realize any tax benefits from its stock option activity or the recognition of stock-based compensation expense because the Company currently has net operating losses and has a full valuation allowance against its deferred tax assets. Accordingly,
Stock Award Modifications
In November 2021, the Company and the former President and CEO mutually agreed to a transition from CEO to a consulting role through June 30, 2022, if not terminated earlier per the terms of the consulting agreement. As a result, the Company modified the terms of its former CEO’s outstanding Stock Awards to (1) automatically vest any unvested stock options or time-based restricted stock units that would have vested in the
The Company determined that vested Stock Awards which had modifications due to the extension of the exercise period were Type 1 modifications pursuant to ASC 718 because those Stock Awards would have vested before and after the modification. Acceleration of vesting for the Stock Awards that would have vested in the
146
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
During the year ended December 31, 2021, total incremental stock compensation expense relating to modifications of stock options and time-based restricted stock units of the former CEO were $
15. Income Taxes
The Company’s benefit from income taxes is as follows:
December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
Current: |
|
|
|
|
|
| |||
Federal | $ | — | $ | — | $ | — | |||
State |
| — |
| ( |
| ( | |||
| — |
| ( |
| ( | ||||
Deferred: |
|
|
|
|
|
| |||
Federal |
| — |
| — |
| — | |||
State |
| — |
| — |
| — | |||
| — |
| — |
| — | ||||
Benefit from income taxes | $ | — | $ | ( | $ | ( | |||
The Company’s tax benefits relate to state R&D tax credits exchanged for cash. The State of Connecticut provides companies with the opportunity to exchange certain R&D credit carryforwards for cash in exchange for foregoing the carryforward of the R&D credit. The program provides for such exchange of the R&D credits at a rate of 65% of the annual R&D credit, as defined. Because the Company’s revenue in 2020 exceeded $70,000, it is not eligible to exchange its 2021 R&D tax credits for cash, therefore there was
A reconciliation of income taxes computed using the U.S. federal statutory rate to that reflected in operations is as follows:
December 31, |
| ||||||
| 2021 |
| 2020 |
| 2019 |
| |
Income taxes using U.S. federal statutory rate |
| | % | | % | | % |
State income taxes, net of federal benefit |
| | % | ( | % | ( | % |
Tax Cuts and Jobs Act |
| | % | | % | | % |
Impact of R&D tax credit on effective tax rate |
| | % | ( | % | | % |
Stock option shortfalls and cancellations |
| ( | % | | % | ( | % |
Permanent items and other |
| ( | % | ( | % | | % |
Change in valuation allowance |
| ( | % | | % | ( | % |
Provision to return |
| | % | | % | ( | % |
Non-taxable revenue |
| | % | | % | | % |
| | % | ( | % | | % | |
147
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Significant components of the Company’s deferred tax assets and liabilities are as follows:
December 31, | ||||||
| 2021 |
| 2020 | |||
Valuation allowance |
| $ | ( |
| $ | ( |
Net operating loss carryforwards | | | ||||
Federal and state tax credits |
| |
| | ||
Deferred revenue |
| — |
| — | ||
Stock-based compensation expense |
| |
| | ||
Other |
| |
| | ||
Deferred tax assets |
| |
| | ||
Other |
| ( |
| ( | ||
Deferred tax liabilities: |
| ( |
| ( | ||
|
| |||||
Net deferred tax asset: | $ | — | $ | — | ||
A
The financial statements reflect expected future tax consequences of such positions presuming the taxing authorities possess full knowledge of the position and all relevant facts. As of December 31, 2021 and 2020, the Company had
At December 31, 2021, the Company had federal and state net operating loss, or NOL, carryforwards of $
In March 2020, former President Trump signed into law the CARES Act (H.R. 748), which was further expanded with the signing of the Consolidation Appropriations Act of 2021 (H.R. 133) on December 27, 2020. The CARES Act (and December expansion) includes a variety of economic and tax relief measures intended to stimulate the economy, including loans for small businesses, payroll tax credits/deferrals, and corporate income tax relief. Due to the Company’s history of tax loss carryforwards and full valuation allowance, the CARES Act did not have a significant effect to the income tax provision, as the corporate income tax relief was directed towards cash taxpayers.
148
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
16. Net (Loss) Income per Share
The Company computes net (loss) income per share in accordance with ASC 260-10, Earnings per Share (see Note 2, Summary of Significant Accounting Policies – (Loss) Income per Share).
The denominators used in the net (loss) income per share computations are as follows:
Year Ended December 31, | ||||||
| 2021 |
| 2020 |
| 2019 | |
Basic: |
|
|
|
|
|
|
Weighted average common shares outstanding |
| |
| |
| |
Diluted: |
|
|
|
|
|
|
Weighted average common shares outstanding - Basic |
| |
| |
| |
Common stock equivalents* |
| |
| |
| |
Denominator for diluted net (loss) income per share |
| |
| |
| |
* | For the year end December 31, 2020, common stock equivalents include dilutive stock options and restricted stock units. For the years ended December 31, 2021 and 2019, |
Basic and diluted net (loss) income per share is computed as follows:
Year Ended December 31, | |||||||||
| 2021 |
| 2020 |
| 2019 | ||||
Net (loss) income - basic and diluted | $ | ( | $ | | $ | ( | |||
Weighted-average common shares outstanding - basic |
| |
| |
| | |||
Effect of dilutive securities: |
|
|
| ||||||
Stock options | — | | — | ||||||
Restricted stock units | — | | — | ||||||
Weighted-average common shares outstanding - diluted | | | | ||||||
Net (loss) income per share: |
|
|
|
|
|
| |||
Basic | $ | ( | $ | | $ | ( | |||
Diluted | $ | ( | $ | | $ | ( | |||
As of December 31, 2021,
As of December 31, 2020,
149
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
As of December 31, 2019,
17. Employee Benefit Plan
The Company’s defined contribution retirement plan complies with Section 401(k) of the Internal Revenue Code.
18. Commitments and Contingencies
License Agreement with Enteris Biopharma, Inc.
In August 2019, the Company entered into the Enteris License Agreement, pursuant to which Enteris granted to the Company a non-exclusive, royalty-bearing license, including the right to grant sublicenses, under certain proprietary technology and patent rights related to or covering formulations for oral delivery of peptide active pharmaceutical ingredients with functional excipients to enhance permeability and/or solubility, known as Enteris’s Peptelligence® technology, to develop, manufacture and commercialize products using such technology worldwide, excluding Japan and South Korea.
As consideration for the licensed rights under the Enteris License Agreement, the Company paid an upfront fee equal to $
The Company is also obligated, pursuant to the Enteris License Agreement, to pay Enteris (1) milestone payments upon the achievement of certain development, regulatory and commercial milestones and (2) low-single digit royalty percentages on net sales of licensed products, subject to reductions in specified circumstances. Until the second anniversary of the entry into the Enteris License Agreement, the Company has the right, but not the obligation, to terminate the Royalty Buyout. The Company did not exercise its Royalty Buyout right and such right expired in August 2021. During the years ended December 31, 2021 and 2020, the Company paid $
The Enteris License Agreement will expire on a country-by-country, licensed product-by-licensed product basis upon the later of (1) the expiration (or invalidation) of all valid claims in licensed patent rights that cover such product in such country, (2) the end of the calendar quarter in which generic competition (as defined in the Enteris License Agreement) occurs for such product in such country and (3)
Either party may terminate the Enteris License Agreement upon written notice if the other party has failed to remedy a material breach within
150
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
for a licensed product in the United States for any indication upon
Manufacturing Agreement with Patheon UK Limited
In July 2021, the Company entered into an API Commercial Supply Agreement with Polypeptide Laboratories S.A., or PPL, that defines each party’s responsibilities with respect to PPL’s manufacture and supply of the active pharmaceutical ingredient difelikefalin, or API, for the difelikefalin injection product candidate. Under the API Commercial Supply Agreement, PPL shall manufacture API at its facility for sale and supply to the Company, in the amounts as set forth in purchase orders to be provided by the Company. The Company will be required to purchase its requirements of API for each year of the term of the agreement, based on internal forecasts.
The API Commercial Supply Agreement will continue until the fifth anniversary of the approval by the FDA of the new drug application for KORSUVA injection, unless the API Commercial Supply Agreement is earlier terminated, and will automatically be extended for successive five-year periods unless either party gives notice to the other party of its intention to terminate.
In July 2019, the Company entered into a Master Manufacturing Services Agreement, or MSA, with Patheon UK Limited, or Patheon. The MSA governs the general terms under which Patheon, or one of its affiliates, will provide non-exclusive manufacturing services to the Company for the drug products specified by the Company from time to time. Pursuant to the MSA, the Company has agreed to order from Patheon at least a certain percentage of its commercial requirements for a product under a related Product Agreement. Each Product Agreement that the Company may enter into from time to time will be governed by the terms of the MSA, unless expressly modified in such Product Agreement.
The MSA has an initial term ending
The MSA contains, among other provisions, customary representations and warranties by the parties, a grant to Patheon of certain limited license rights to the Company’s intellectual property in connection with Patheon’s performance of the services under the MSA, certain indemnification rights in favor of both parties, limitations of liability and customary confidentiality provisions.
Also in July 2019, the Company entered into
151
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
the Monza, Italy and Greenville, North Carolina manufacturing sites, respectively, from API supplied by the Company. Patheon and Patheon Greenville will be responsible for supplying the other required raw materials and packaging components and will also provide supportive manufacturing services such as quality control testing for raw materials, packaging components and finished product.
Leases
The Company’s Stamford Lease had an initial term ending in and is renewable for
In connection with the signing of the Stamford Lease, the Company entered into a standby letter of credit agreement which serves as a security deposit for the Premises. The standby letter of credit is
In June 2020, the Company entered into an amendment to the Stamford Lease to add additional office space, or the Lease Amendment. The term of the Lease Amendment began when renovation of the additional space was completed and the Company took possession of the additional space in October 2020, or the Amendment Commencement Date, and ends on
The rent for the Lease Amendment is at market rate as of the signing of the Lease Amendment. The Lease Amendment requires monthly lease payments, including rent escalations, during the lease term. The Company began paying rent for the Lease Amendment on the Amendment Commencement Date.
In October 2020, the Company recorded an operating lease liability of $
Under ASC 842, lease expenses on the Stamford lease and Lease Amendment are recognized on a straight-line basis over the lease term. As a result, $
Other information related to the Stamford Lease and Lease Amendment was as follows:
Year Ended December 31, | |||||||
| 2021 |
| 2020 | ||||
Cash paid for amounts included in the measurement of lease liabilities: |
|
|
| ||||
Operating cash outflows relating to operating leases | $ | | $ | | |||
ROU assets obtained in exchange for new operating lease liabilities | $ | — | $ | | |||
Remaining lease term - operating leases (years) |
|
| |||||
Discount rate - operating leases | | % | | % | |||
152
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
Future minimum lease payments under the non-cancellable operating leases for the Stamford lease and the Lease Amendment, as well as a reconciliation of these undiscounted cash flows to the operating lease liabilities as of December 31, 2021, were as follows:
Year Ending December 31, |
| ||
2022 |
| $ | |
2023 |
| | |
Total future minimum lease payments, undiscounted |
| | |
Less imputed interest |
| ( | |
Total | $ | | |
Operating lease liabilities reported as of December 31, 2021: |
|
| |
Operating lease liabilities - current | $ | | |
Operating lease liabilities - non-current |
| | |
Total | $ | |
19. Legal Matters
From time to time, the Company may become subject to arbitration, litigation or claims arising in the ordinary course of its business. The Company is not currently a party to any arbitration or legal proceeding that, if determined adversely to the Company, would have a material adverse effect on its business, operating results or financial condition. The results of any future claims or proceedings cannot be predicted with certainty, and regardless of the outcome, litigation can have an adverse impact on the Company because of defense and settlement costs, diversion of management resources and other factors.
20. Related Party Transactions
As of December 31, 2021, Vifor owned
Sales of KORSUVA injection to Vifor for $
21. Subsequent Events
On March 1, 2022, the Company filed a universal shelf registration statement, or the Shelf Registration Statement, which provides for aggregate offerings of up to $
153
CARA THERAPEUTICS, INC.
NOTES TO FINANCIAL STATEMENTS
(amounts in thousands, except share and per share data)
securities that had been registered under the Company’s previous Registration Statement on Form S-3 (File No. 333-230333) that was declared effective on April 4, 2019.
The Company may offer additional securities under its Shelf Registration Statement, when declared effective, from time to time in response to market conditions or other circumstances if it believes such a plan of financing is in the best interests of its stockholders. On March 1, 2022, the Company entered into an open market sales agreement, or the Sales Agreement, with Jefferies LLC, as sales agent, pursuant to which it may, subject to the effectiveness of the Shelf Registration Statement, from time to time, issue and sell common stock with an aggregate value of up to $
154
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure.
None.
Item 9A. Controls and Procedures.
Evaluation of Disclosure Controls and Procedures
Our management, with the participation of our Chief Executive Officer and Chief Financial Officer, has evaluated the effectiveness of our disclosure controls and procedures (as such term is defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act) as of December 31, 2021. Based on such evaluation, our Chief Executive Officer and Chief Financial Officer have concluded that, as of December 31, 2021, our disclosure controls and procedures were effective to provide reasonable assurance that information required to be disclosed by us in the reports that we file or submit under the Exchange Act is (1) recorded, processed, summarized, and reported within the time periods specified in the rules and forms of the SEC, and (2) accumulated and communicated to our management, including our principal executive officer and principal financial officer, as appropriate to allow timely decisions regarding required disclosures.
Management’s Report on Internal Control over Financial Reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting as defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act. Our internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Our management utilized the criteria established in the Internal Control – Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO) to conduct an assessment of the effectiveness of our internal control over financial reporting as of December 31, 2021. Based on the assessment, management has concluded that, as of December 31, 2021, our internal control over financial reporting was effective.
Ernst & Young LLP, an independent registered public accounting firm, has audited the effectiveness of our internal control over financial reporting as of December 31, 2021, as stated in their attestation report, which is included in Part II Item 8 of this Annual Report.
Changes in Internal Control Over Financial Reporting
There were no changes in our internal control over financial reporting that occurred during the quarter ended December 31, 2021 that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting.
Limitations on Controls and Procedures
Management, including our Chief Executive Officer and Chief Financial Officer, recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving their objectives and management necessarily applies its judgment in evaluating the cost benefit relationship of possible controls and procedures. Because of the inherent limitations in all control systems, no evaluation of controls and procedures can provide absolute assurance that all control issues and instances of fraud, if any, within Cara have been detected.
Item 9B. Other Information.
None.
155
Item 9C. Disclosure Regarding Foreign Jurisdictions that Prevent Inspections.
Not applicable.
PART III
Item 10. Directors, Executive Officers and Corporate Governance.
The information required by this item will be set forth under the captions “Executive Officers”, “Election of Directors” and “Board of Directors and Corporate Governance” in our Definitive Proxy Statement with respect to our 2022 Annual Meeting of Stockholders and is incorporated herein by reference.
Item 11. Executive Compensation.
The information required by this item will be set forth under the captions “Executive Compensation” and “Board of Directors and Corporate Governance” in our Definitive Proxy Statement with respect to our 2022 Annual Meeting of Stockholders and is incorporated herein by reference.
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters.
The information required by this item will be set forth under the captions “Security Ownership of Certain Beneficial Owners and Management” and “Securities Authorized for Issuance under Equity Compensation Plans” in our Definitive Proxy Statement with respect to our 2022 Annual Meeting of Stockholders and is incorporated by reference.
Item 13. Certain Relationships and Related Transactions and Director Independence.
The information required by this item will be set forth under the captions “Transactions with Related Persons” and “Board of Directors and Corporate Governance” in our Definitive Proxy Statement with respect to our 2022 Annual Meeting of Stockholders and is incorporated herein by reference.
Item 14. Principal Accountant Fees and Services.
The information required by this item will be set forth under the caption “Independent Registered Public Accounting Firm’s Fees” in our Definitive Proxy Statement with respect to our 2022 Annual Meeting of Stockholders and is incorporated herein by reference.
156
PART IV
Item 15. Exhibits, Financial Statement Schedules.
(a) We have filed the following documents as part of this Annual Report on Form 10-K:
(1) Financial Statements of Cara Therapeutics, Inc.
INDEX TO FINANCIAL STATEMENTS
PAGE | |
101 | |
Financial Statements: | |
104 | |
105 | |
106 | |
107 | |
108 |
(2) Financial Statement Schedules
All schedules for which provision is made in the applicable accounting regulations of the SEC which are not included with this additional financial data have been omitted because they are not applicable or the required information is shown in the Financial Statements or Notes included in Item 8. Financial Statements and Supplementary Data.
(3) List of Exhibits
Incorporated by Reference | ||||||||||
Exhibit |
| Description of Exhibit |
| Form |
| File No. |
| Exhibit No. |
| Date Filed |
3.1 | 8-K | 001-36279 | 3.1 | February 7, 2014 | ||||||
3.2 | 8-K | 001-36279 | 3.2 | February 7, 2014 | ||||||
4.1 | S-1/A | 333-192230 | 4.1 | January 17, 2014 | ||||||
4.2# | S-3ASR | 333-233666 | 4.3 | September 9, 2019 | ||||||
4.3 | 10-K | 001-36279 | 4.3 | February 27, 2020 | ||||||
4.4# | 10-K | 001-36279 | 4.4 | February 25, 2021 | ||||||
10.1+ | S-1/A | 333-192230 | 10.1 | January 17, 2014 | ||||||
10.2+ | S-1/A | 333-192230 | 10.3 | January 17, 2014 | ||||||
157
10.2.1 | Form of Stock Option Agreement under 2014 Equity Incentive Plan. | S-1/A | 333-192230 | 10.3.1 | January 17, 2014 | |||||
10.2.2 | Form of Restricted Stock Unit Award under 2014 Equity Incentive Plan. | S-1/A | 333-192230 | 10.3.2 | January 17, 2014 | |||||
10.3* | S-1 | 333-192230 | 10.7 | November 8, 2013 | ||||||
10.4* | S-1 | 333-192230 | 10.8 | November 8, 2013 | ||||||
10.5 | S-1 | 333-192230 | 10.9 | November 8, 2013 | ||||||
10.6# | API Commercial Supply Agreement between Cara Therapeutics, Inc. and Polypeptide Laboratories S.A. | 10-Q | 001-36279 | 10.1 | November 8, 2021 | |||||
10.7+ | 8-K | 001-36279 | 10.1 | November 3, 2021 | ||||||
10.8+ | 8-K | 001-36279 | 10.1 | February 7, 2014 | ||||||
10.9+ | 8-K | 001-36279 | 10.2 | November 3, 2021 | ||||||
10.10+ | 8-K | 001-36279 | 10.2 | February 7, 2014 | ||||||
10.11+ | 10-K | 001-36279 | 10.11 | March 12, 2019 | ||||||
10.12+ | 8-K | 001-36279 | 10.1 | October 1, 2020 | ||||||
10.13†+ | ||||||||||
10.14†+ | Cara Therapeutics, Inc. Severance Plan and Form of Participation Agreement | |||||||||
10.15+ | Amended and Restated Non-Employee Director Compensation Policy. | 10-Q | 001-36279 | 10.1 | May 11, 2020 | |||||
10.16 | Lease Agreement dated December 21, 2015 between the Registrant and Four Stamford Plaza Owner L.L.C. | 8-K | 001-36279 | 10.1 | December 23, 2015 |
158
10.17 | 10-Q | 001-36279 | 10.2 | August 10, 2020 | ||||||
10.18* | 10-Q | 001-36279 | 10.1 | August 7, 2018 | ||||||
10.19# | 10-Q | 001-36279 | 10.2 | August 7, 2019 | ||||||
10.20# | 10-Q | 001-36279 | 10.1 | November 5, 2019 | ||||||
10.21+ | 8-K | 001-36279 | 10.1 | November 20, 2019 | ||||||
10.22 | Form of Stock Option Grant Notice under 2019 Inducement Plan | 8-K | 001-36279 | 10.2 | November 20, 2019 | |||||
10.23 | Form of Restricted Stock Unit Notice under 2019 Inducement Plan | 8-K | 001-36279 | 10.3 | November 20, 2019 | |||||
10.24# | 10-K | 001-36279 | 10.21 | February 25, 2021 | ||||||
23.1† | Consent of Ernst & Young, LLP, independent registered public accounting firm. | |||||||||
24.1† | ||||||||||
31.1† | ||||||||||
31.2† | ||||||||||
159
32.1†** | ||||||||||
101.CAL† | Inline XBRL Taxonomy Extension Calculation Linkbase. | |||||||||
101.INS† | Inline XBRL Instance Document. | |||||||||
101.LAB† | Inline XBRL Taxonomy Extension Label Linkbase. | |||||||||
101.PRE† | Inline XBRL Taxonomy Extension Presentation Linkbase. | |||||||||
101.SCH† | Inline XBRL Taxonomy Extension Schema Linkbase. | |||||||||
101.DEF† | Inline XBRL Taxonomy Extension Definition Linkbase Document. | |||||||||
104† | Cover page interactive data file (formatted as Inline XBRL and contained in Exhibit 101). |
+ | indicates management contract or compensatory plan. |
* | Confidential treatment has been granted with respect to certain portions of this exhibit. Omitted portions have been filed separately with the Securities and Exchange Commission. |
# | Portions of this exhibit (indicated by asterisks) have been omitted because the Registrant has determined they are not material and are the type that the Registrant treats as private and confidential. |
† | Filed herewith. |
** | This certification is deemed not filed for purposes of Section 18 of the Securities Exchange Act of 1934, as amended, or otherwise subject to the liability of that section, nor shall it be deemed incorporated by reference into any filing under the Securities Act of 1933, as amended, or the Securities Exchange Act of 1934, as amended. |
Item 16. Form 10-K Summary.
Not applicable.
160
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized on this 1st day of March 2022.
CARA THERAPEUTICS, INC. | ||
By: | /s/ CHRISTOPHER POSNER | |
Name: | Christopher Posner | |
Title: | President and Chief Executive Officer | |
KNOW ALL PERSONS BY THESE PRESENTS, that each person whose signature appears below constitutes and appoints Christopher Posner and Scott Terrillion, and each of them, as his true and lawful attorneys-in-fact and agents, with full power of substitution for him, and in his name in any and all capacities, to sign any and all amendments to this Annual Report on Form 10-K, and to file the same, with exhibits thereto and other documents in connection therewith, with the U.S. Securities and Exchange Commission, granting unto said attorneys-in-fact and agents, and each of them, full power and authority to do and perform each and every act and thing requisite and necessary to be done therewith, as fully to all intents and purposes as he might or could do in person, hereby ratifying and confirming all that said attorneys-in-fact and agents, and either of them, his substitute or substitutes, may lawfully do or cause to be done by virtue hereof.
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
Signature |
| Title |
| Date |
/s/ CHRISTOPHER POSNER | President, Chief Executive Officer | March 1, 2022 | ||
Christopher Posner | (Principal Executive Officer) | |||
/s/ THOMAS REILLY | Chief Financial Officer | March 1, 2022 | ||
Thomas Reilly | (Principal Financial and Accounting Officer) | |||
/s/ MARTIN VOGELBAUM | Director | March 1, 2022 | ||
Martin Vogelbaum | ||||
/s/ HARRISON M. BAINS, JR. | Director | March 1, 2022 | ||
Harrison M. Bains, Jr. | ||||
/s/ JEFFREY IVES | Director | March 1, 2022 | ||
Jeffrey Ives, Ph.D. | ||||
/s/ SUSAN SHIFF | Director | March 1, 2022 | ||
Susan Shiff, Ph.D. |
161
Serious News for Serious Traders! Try StreetInsider.com Premium Free!
You May Also Be Interested In
- Crexendo Growth Surges with Four and a Half Million Users on its Software Platform With Platform Growing At Nearly Twice The Industry Average
- LQWD Files Final Base Shelf Prospectus
- Visited App Publishes Top 25 Most Visited Cruise Ports in the World
Create E-mail Alert Related Categories
SEC FilingsSign up for StreetInsider Free!
Receive full access to all new and archived articles, unlimited portfolio tracking, e-mail alerts, custom newswires and RSS feeds - and more!


 Tweet
Tweet Share
Share